By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

March 3, 2021
New E/M codes went into effect at the beginning of this year. Now that we are a couple of months into using the new definitions for the E/M codes, here are the lessons we should have learned.
REIMBURSEMENT
Let’s start with reimbursement for the medical eye examination codes. Here’s the path to see the Medicare Physician Fee Schedule:
Overview of the Medicare Physician Fee Schedule Search | CMS
Click Begin Search or follow this path: License for Use of Current Procedural Terminology, Fourth Edition (“CPT”) | CMS
Click Accept.
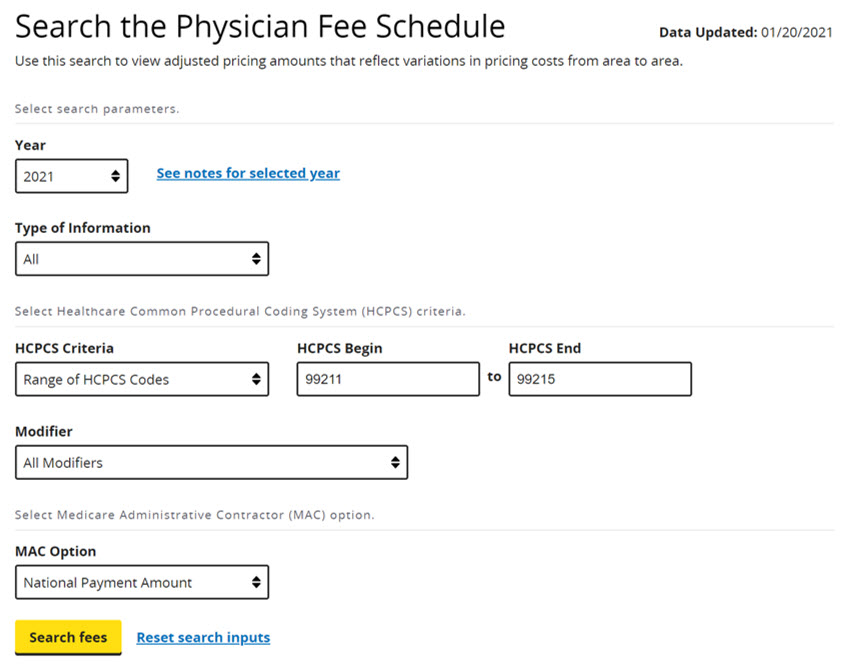
Enter the search parameters for the codes you wish to see. Here’s an example you would use for the range of codes from 99211-99215 (change this to see any CPT code or code range) for the year 2021 (change this for any year you want to see) for the National Payment Amount (change this option to see your specific location amount).
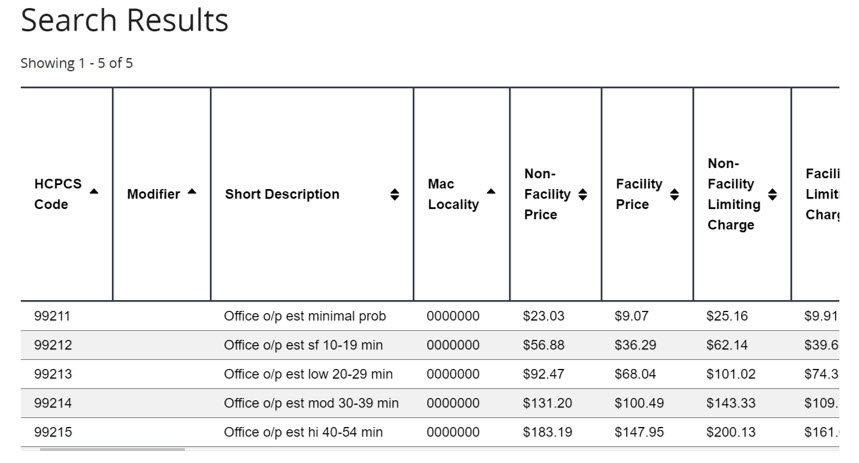
When you click Search Fees, you get this screen:
With this background you can assemble the following chart for the code you would use for eye examinations.
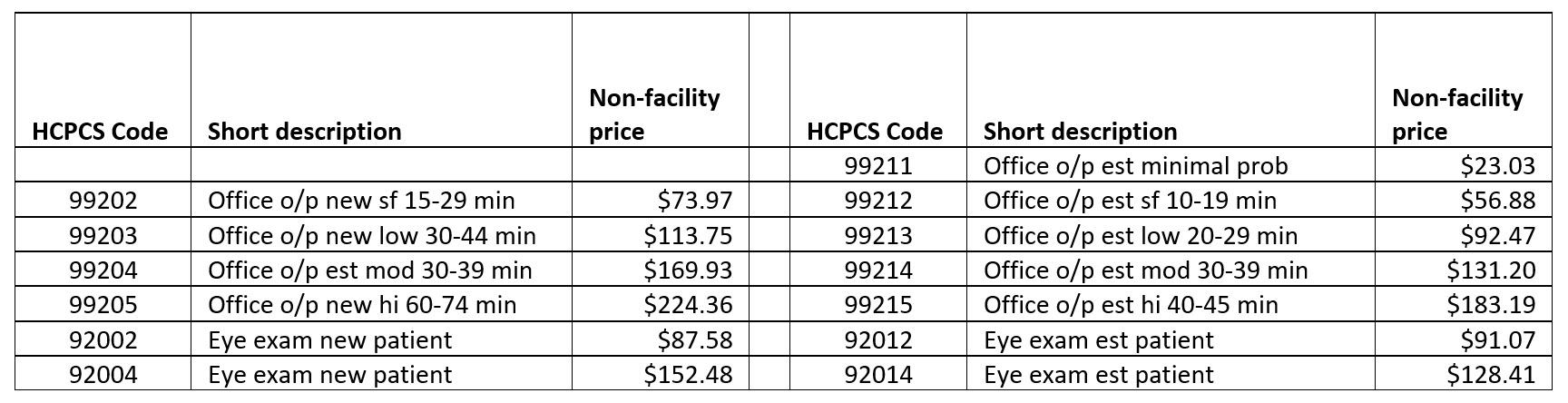
Note that the 99201 code has been deleted. It was a rarely used code. Note also that 99211 continues to exist. However, because it’s the only code that can be billed by as a non-doctor service, it really isn’t that significant.
With the knowledge we’ve gained from the chart above, let’s ask a question. What is your comprehensive exam fee? If it is $153 or more, then you will not leave any money on the table with the 92000 eye exam codes, but if you could bill 99204, then your exam needs to be billed at $170 or more to be in the same situation.
Remember that you cannot have multiple fees for the same CPT code. Bill everyone the same for the same CPT code.
For completeness, you should repeat this reimbursement exercise across all third parties for which you are provider.
The change in coding level requirements for the 99000 series codes is important to note. However, remember that you still must document what is “medically appropriate.” You must document what is needed to support the diagnosis of any condition that you determine on the patient visit.
Other Articles to Explore
TIME
Another change to note is that billing via time for the 99000 codes means that you need to document the time spent in the patient examination. Both face-to-face time and non-face-to-face time counts. That’s true unless there are CPT codes being separately billed for this exam. For example, if the doctor spends a total of 25 minutes in the patient examination today, but five minutes of that time is spent looking at OCT and Visual Fields testing that will also be billed today, then the doctor can only bill for 20 minutes of exam time.
The 92000 eye exam codes do not have a time option.
DECISION-MAKING CODING
Within the new system for E/M coding based on decision-making there are three areas: Problems, Data and Management to consider. Most doctors are using Problems and Management to choose a code level. Since the new rule is “2 of 3,” this is acceptable.
ACTION PLAN
Take this week to review your coding and billing protocols. Be sure to look at these three areas: Reimbursement, Time and Decision-Making Coding. Make any adjustments necessary in order to be compliant with the new rules.



























