Victoria Dzurinko, OD, MBA, FAAO
Dec. 30, 2020
It’s been said that if no one ever got sick or injured, primary health-care providers would be out of work. That’s not quite accurate, especially for optometrists. And healthy businesses are the result of our success at building lasting relationships by maintaining our patients’ quality of life.
Evolving practice demographics—whether patients are older or younger—will continue to influence the extent to which it’s possible to position a practice around wellness and preventative care. If your practice is like mine was, you are probably noticing a growing number of patients requiring more complex care, and your investments in technology will likely be dictated by their specific needs.
The ever-increasing constraints on our time and resources is a challenge that’s not easily resolved as we add more medical eyecare to the practice. But there is a condition that all optometrists are empowered to manage to both impact patients’ lives and build stronger, more profitable practices : age-related macular degeneration (AMD)1. I am excited to show you how AMD is one of optometry’s biggest opportunities to provide enhanced care to patients starting from the earliest symptom of night vision difficulties to the day we may need to make the critical, vision-saving referral for intravitreal injections.
Why We Hate AMD Management
As clinicians, we think about AMD every day. We don’t want our patients to lose vision while under our care—and we don’t want to jeopardize our business by missing something or failing to refer. Patients present with drusen that can be hard to detect and, when discovered, have clinically ambiguous meaning at diagnosis. We worry because, particularly with AMD, we are often caught by surprise with what appears to be sudden and rapid progression of what we thought was mild or early disease.
Can we predict the future for our AMD patients? If you asked me that question five or six years ago, I would have said “no.” But dark adaptation technology has completely changed our ability to diagnose and manage early and intermediate AMD with confidence and ease. Impaired dark adaptation is the first clinical biomarker for AMD and may precede the visible presentation of drusen. In fact, this functional test not only enables us to detect subclinical AMD with 90 percent accuracy at least three years before it can be observed clinically2 , but it also enables us to better monitor progression of the disease by carefully watching for both functional and clinical signs of deterioration.
Importantly, the Rod Intercept (RI) score, as measured by the AdaptDx dark adaptometers, allows us to secure patient buy-in with critical lifestyle changes like smoking cessation. By assigning AMD an easy-to-understand value, much like an IOP or A1c, patients are often more willing to comply with our therapeutic plan along with a more frequent follow-up schedule.3 Furthermore, offering a true AMD diagnosis (versus hypothetical conversations about risk) helps reinforce supplementation recommendations and other interventions.
Patients Win with AMD Management
With the addition of dark adaptation testing to our practices, we can make a real difference in patients’ lives. AMD is more prevalent than glaucoma and diabetic retinopathy combined, and most patients are in the early to intermediate stages of disease. That puts the ball squarely in optometry’s court. But what should we do with it? Before dark adaptation was available, many of us had no choice but to sit back helplessly and just watch the clock run out for our patient’s vision. But now, we’re pushing the game into overtime and we’re in it to win the battle against the blindness caused by AMD.
Intravitreal injection (anti-VEGF) has become one of the most commonly performed procedures in the U.S. within any field of medicine.4, 5, 6 But by the time a patient reaches this stage, significant damage and vision loss has likely already occurred. With dark adaptation testing, optometrists are at the ready, prepared to identify and monitor earlier stage disease. We now know whether OCT scans and other tests are indicated. And although lifestyle changes, diet and exercise modification, systemic disease management, nutritional supplementation, retinal light protection, and more careful follow-up, will not cure AMD, they have each been shown to slow or even halt the progression of the disease.7
Practices Win with AMD Management
Nearly all of us in private practice come to realize that when we do what’s good for our patients, it tends to be good for our practices. This applies to AMD as well. Since transitioning from private practice to my role as director of professional relations for MacuLogix, I’ve had the opportunity to speak with many of our AdaptDx users. They often tell me that no matter how they implement dark adaptation testing—whether it be a wellness screening model testing all patients over a certain age or a medical model focused on testing patients with findings such as drusen or night blindness—their practices have benefited greatly. They have seen a revenue increase not just from dark adaptation testing, but from additional imaging, more frequent follow-up appointments, and increased optical and nutraceutical sales.
Other Articles to Explore
Several colleagues, including Jeffry Gerson, OD, and Gary Kirman, OD, have shared that annual per patient revenue can go from approximately $150 to $500 or more once a patient is diagnosed with AMD. And thanks to dark adaptation, they are uncovering more patients with AMD years before they can see it clinically. In their practices, catching the disease as early as possible leads to more loyal and appreciative patients who know they are getting the best possible care.
We also worked with a two-clinic practice in the Midwest to measure the financial impact of dark adaptation testing over an eight-month period, compared to the previous year. Honestly, the results even surprised me. These two clinics reported more than $52,000 in additional revenue from dark adaptation testing and related increases in OCT usage and nutraceutical sales, as follows:
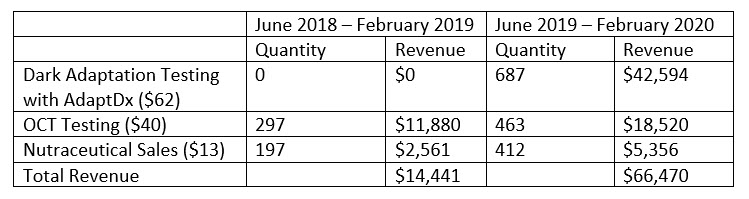
In addition, these two clinics recommend high energy visible light (HEVL) protection for each AMD patient and reported a 146 percent increase in HEVL sales during this same period, driving a significant revenue boost in optical. These practices are proving that what is good for the patient is indeed good for the practice.
Don’t Miss the Second Half
The original AdaptDx automated dark adaptometer was introduced in 2014 and is now widely used in optometric practice. But this year, I’m proud to say that MacuLogix, my employer, introduced an even easier way to measure dark adaptation, using a self-contained wearable headset called the AdaptDx Pro. An artificial intelligence-driven, on-board technician named Theia increases the likelihood of a consistent testing experience and reliable results. After your technician selects the testing protocol and places the device on the patient, Theia administers the test from start to finish. Patients can take the AdaptDx Pro test anywhere in the office, in any light.
Importantly, the medical-grade hardware withstands all necessary disinfection and the hygienic barrier that makes contact with the patient’s face is designed for single use, offering a greater level of patient confidence in this new era of point-of-care testing.
As optometrists navigate historical changes in life and in practice, there are some silver linings. There is greater opportunity to improve both patient outcomes and our practice bottom lines by integrating dark adaptation testing in the identification and management of AMD. Most notably, we can erase much of the uncertainty of AMD, while safeguarding the health of our patients, and realizing the fiscal rewards made possible with dark adaptation technology.
References
1. Lowe PA. When Opportunity Knocks. In: Practical Opportunities in AMD Management. Review of Optometry, September 15, 2020.
2. Jackson GR, Scott IU, Kim IK, Quillen DA, Iannaccone A, Edwards JG. Diagnostic sensitivity and specificity of dark adaptometry for detection of age-related macular degeneration. Investigative Ophthalmology & Visual Science. 2014;55(3):1427-31.
3. Gerson J. Dark Adaptation Is Proven to Find Treatable AMD. In: Practical Opportunities in AMD Management. Review of Optometry, September 15, 2020.
4. Chiang MF. How Does the Standard of Care Evolve? Anti-Vascular Endothelial Growth Factor Agents in Retinopathy of Prematurity Treatment as an Example. Ophthalmology. 2018;125(10):1485-1487.
5. Parikh R, Ross JS, Sangaralingham LR, Adelman RA, Shah ND, Barkmeier AJ. Trends of Anti-Vascular Endothelial Growth Factor Use in Ophthalmology Among Privately Insured and Medicare Advantage Patients. Ophthalmology. 2017;124(3):352-358.
6. Atchison EA, Wood KM, Mattox CG, Barry CN, Lum F, MacCumber MW. The Real-World Effect of Intravitreous Anti-Vascular Endothelial Growth Factor Drugs on Intraocular Pressure: An Analysis Using the IRIS Registry. Ophthalmology. 2018;125(5):676-682.
7. Lowe PA. When Opportunity Knocks. In: Practical Opportunities in AMD Management. Review of Optometry, September 15, 2020.
 Victoria Dzurinko, OD, MBA, FAAO, is the director of professional relations for MacuLogix. To contact her: vdzurinko@maculogix.com
Victoria Dzurinko, OD, MBA, FAAO, is the director of professional relations for MacuLogix. To contact her: vdzurinko@maculogix.com





















