By David Geffen, OD, FAAO

June 28, 2017
Cataract surgery is one of the the most common surgeries performed in the world, and optometrists are in a prime position to help make those surgeries a success. As optometrists, we don’t perform the surgeries, but we work with patients before and after.
How well we set expectations, and educate patients about all of their options, including premium multifocal IOLs, determines how likely the patient is to be satisfied with their surgery, and how likely they are to remain in our practice. It’s important to educate on the importance of total eye health, and not just visual acuity.
Most surgery centers see their one-day cataract post-ops, and then refer the patient back to the OD’s office for the balance of post-operative care. For standard cataracts, versus premium IOLs, like multifocals or torics, the post-op global period is 90 days, and is reimbursed at 20 percent of the Medicare-approved fee. This is approximately $100.
If the patient receives a premium IOL, the surgical fee to the patient may be $1,000-$3,000 per eye, depending on the exact circumstances. The co-management fees typically will be for one year, and approximately 20 percent of the surgeon’s fees. The higher fees reflect the additional work and time you will put into taking care of these patients.
I practice in a shared OD-MD practice, and we make sure cataract patients fully understand what the surgery will do for their vision, and how their optometrist can best work with their surgeon to create a good outcome. Patients who are satisfied with their surgery are patients who more likely to return to the OD who guided them through it.
Provide Education to Patients
If the referring optometrist doesn’t educate the patient, that patient may end up getting an IOL that won’t meet their vision needs and expectations. For instance, if the patient is wearing multifocal contact lenses, then they will most likely want a multifocal IOL. The OD should say to the patient: “Mrs. Smith, you have been wearing multifocal contacts for the past 10 years, so I am recommending that you ask your surgeon about the new multifocal IOLs, which I think will make you very happy.”
Now, when Mrs. Smith goes to the surgery center, and the surgeon recommends a multifocal IOL, she will say, “Oh, yes, my optometrist told me about those,” and it no longer will look like the surgeon is just selling her something.
It is also important to talk briefly about the process to show that even though you are not participating in the surgery, you will be taking care of the post-op visits, and that you are a part of the team that will ensure the surgery is a success. Doing so helps patients understand the co-management arrangement, and helps keep your patients coming back. Plus, making sure the surgery center and your office speak as one instills confidence in the patient, and builds long-term trust.
Just as you educate patients about premium IOL options, such as multifocal IOLs, you also should explain how today’s IOLs can accommodate the needs of patients with visual conditions such as astigmatism. We would never fit a 2 diopter astigmat with spherical soft lenses, so why do we not tell the patient about toric IOL’s?
If the patient has over 1.00D of corneal astigmatism, we know that there will be residual cylinder if we do not address this at the time of surgery. We need to educate the patient, so when they go to the surgery center, and the surgeon talks about astigmatism, they don’t think it’s just an up-sell, but in their best interest.
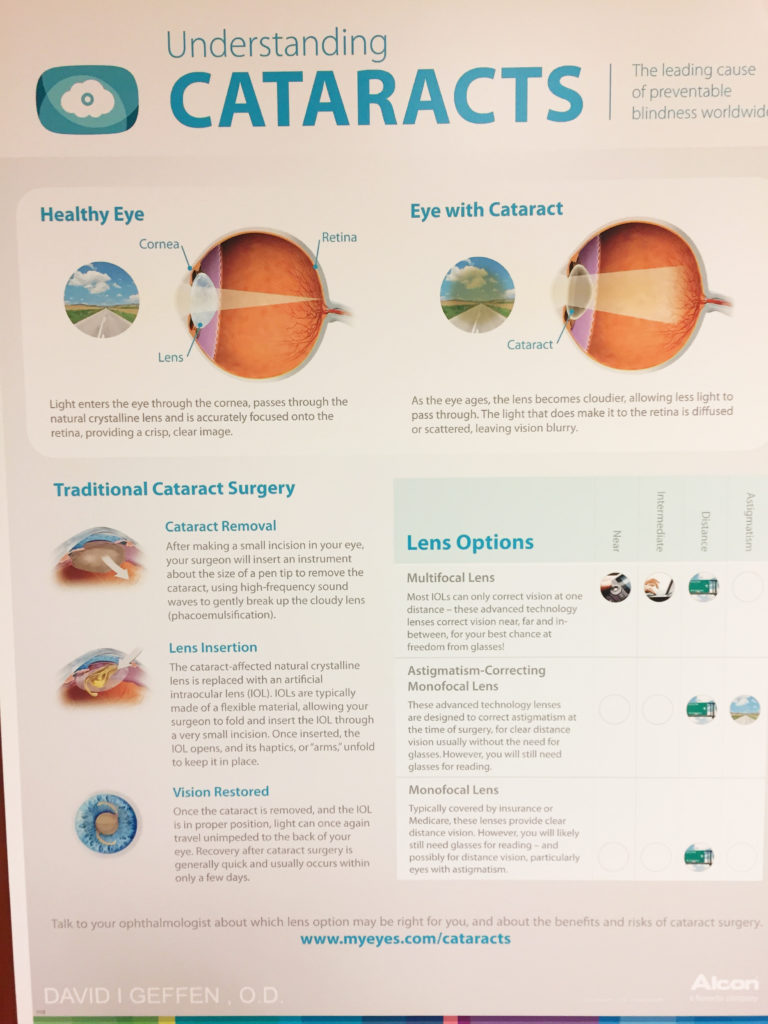
An educational poster about cataract surgery, including the premium IOL options available. Dr. Geffen says the education the co-managing OD provides relates directly to the level of satisfaction the patient feels following the procedure.
I tell my patients that the astigmatism they have had for many years can be corrected with cataract surgery. I might say: “We have many excellent IOLs, which should provide you with excellent distance vision. You may still need spectacles for certain things, like near work, but we can even address that need today with advanced technology.”
Another essential part of patient education is helping the patient to set realistic expectations. Most patients think cataract surgery will make them 30 again, and do not realize they will still need near correction. We tell our patients that generally they can expect excellent distance acuity with the surgery, but that if they have over 1D of astigmatism, we say that the lens will not correct for this, and I recommend a more advanced procedure to eliminate this, so the distance vision will be optimized. I tell them that this will cost a little more than what is covered, but it is a once-in-a-lifetime decision.
I go on to say: “We even have lenses today that may help with your near vision, and reduce the need for near correction, but for certain activities, you may still want reading glasses to make it easier.” I may also demonstrate what their vision would be like without a near add if their acuity is still good enough. I would say: “Some of these lenses will have trade offs just like your glasses or contacts; it’s all a mater of getting you the best lens for your lifestyle.”
You can cap off your patient education by providing patients with written, or online, information to help them remember what you told them, and to offer additional information. Most of the IOL companies will provide handouts and other educational material for your office.
You can go online to request these, or request them of an IOL sales rep. There also are several web sites with excellent information about cataract surgery. These include: thinkaboutyoureyes.com, allaboutvision.com and technis.com.
After the one year of post-op care, be sure to tell the patient they still need their regular eye exams to ensure the health of their eyes. They need to know that problems such as glaucoma and macular degeneration are screened for at annual exams, and are best treated early.
Effectively Co-Manage
It is important to make sure your office knows the post-operative instructions given to the patient from the surgery center, so you can reinforce compliance, and also to not look stupid in the patient’s eyes by giving them conflicting information. In my office, if we deviate from the established post-op protocol, we explain to the patient why we are doing this.
To familiarize yourself with the cataract surgery process, from the surgeon’s perspective, I recommend spending a half-day with a surgeon seeing post-op appointments. Then you will be able to tell your patients exactly what to expect at the surgeon’s office.
Communication is critical between the optometrist’s office and the surgery center. The center should provide a prompt report after the initial consultation, and then after surgery, to explain to the referring doctor exactly what has transpired and what IOL was used. The optometrist should provide a pre-operative report explaining the typical vision demand of the patient and their current vision correction needs.
For example, if monovision has been used for years, the surgeon needs to know this. If the patient has been sensitive to any disruption of distance vision, this too needs to be communicated. After each visit a report should be sent to the surgeon. The center needs this data for their outcomes to improve care for future patients.
Most centers have forms, which are quick and easy to fill out, but just sending a summary from your EHR is typically fine. The center should be willing to take phone calls and discuss concerns with you. Keep in mind that all communication about patients should take place via HIPAA-compliant platforms, such as from your EHR to theirs.
There are no shortage of surgery centers looking for your business. You should have a good working relationship with the surgeons, as well as their support staff. Communication is vital to the trust of each doctor and patient. Fair fees are important, but just going with the highest may not be the best for your patients, and if it is not the best for your patient, it will come back to haunt you.
Do your research, including finding out the technology the center is using for the surgery, along with the personalities of the surgeon and their staff, and vitally important, how many cataract surgeries they have conducted, and what the outcomes were of the majority of those surgeries.
 David I. Geffen, OD, FAAO, is a partner in Gordon Schanzlin New vision-TLC in La Jolla, Calif. Contact: dig2020@aol.com
David I. Geffen, OD, FAAO, is a partner in Gordon Schanzlin New vision-TLC in La Jolla, Calif. Contact: dig2020@aol.com



























