Sponsored Content

Moderated by Sally M. Dillehay, OD, EdD
Sept. 16, 2020
We were expecting 2020 to be the year highlighting our essential role in primary healthcare. Instead, it quickly became the year of COVID-19. The pandemic still leaves many questions, including how best to incorporate Personal Protective Equipment (PPE) into our practices moving forward.
To provide the safest experience for patients, it is critical to understand the risks of the COVID-19 outbreak, and incorporate best practices to protect the health and well-being of those who entrust us with their eye and health care. I recently sat down with a group of eyecare leaders to discuss the challenges and some best practices to not just survive, but thrive during these uncertain times.

Business Impact
Dr. Dillehay: Approximately six months into dealing with COVID-19, what has been the impact on your business?
Maurice Wilson, OD: April was pretty slow with only emergency care offered. As Texas opened up, business came back quickly. We are now 90-95 percent on track for the year.
R. Max Raynor, OD: During the early months, we only provided medically necessary care, and were at about 30 percent of capacity. Now, we are busier than ever, even greater than pre-COVID, and are struggling to meet demand.
Amanda Nanasy, OD: The “shutdown” and need to re-imagine patient care and team member utilization has forced us to improve our processes with better and more consistent communications. Our patients have been vocal about how impressed they are with our changes. Although we are down in overall revenue, we are far exceeding revenue per patient.
Practice Impact
Dr. Dillehay: As Dr. Nanasy points out, reinventing our practices is critical when leading through a crisis. What are some other changes you made to help manage the impact of the pandemic on your practice?
Dr. Raynor: We ask standard COVID questions and take temperatures upon arrival. Case histories are taken over the phone. We are implementing telemedicine. Our staff is disinfecting each room after use. We consistently wash hands after close contact. We have baskets that patients use for frames, and disinfect every frame with UV light.
George D. Shida, OD: We schedule fewer patients per hour, and increased cleaning and disinfection protocols. Staff are all cross-trained in case of unplanned extended absences.
Julie Schornack, OD, MEd: Like Dr. Nanasy, we enhanced all of our communications. We found most people did well wearing masks and washing hands; however, social distancing is a bigger challenge. We created a distinctive graphic for signage everywhere. We added a significant amount of detailed information to our web site about COVID-19.

Courtesy of Marshall B. Ketchum University
Dr. Dillehay: In a Jobson survey (Coronavirus ECP Study, Wave 14, August 21-25), 86 percent of ECPs saw frontline or essential workers who may have had contact with infected people; 16 percent reported someone at their location tested positive for COVID-19. How do you see PPE protocols changing in the years ahead?
Dr. Raynor: Even once there is an effective vaccine or treatments, we will continue to maintain strong PPE protocols.
Dr. Shida: EKC, influenza and COVID-19 asymptomatic patients can present at any time. In the future, we will still be uncertain if a patient is infectious or not, and PPE will still be required.
Dr. Schornack: For the foreseeable future, PPE is here to stay. It will likely be helpful for other respiratory based infections such as influenza.
PPE Learnings
Dr. Dillehay: Are there any other learnings or pearls of wisdom you can share regarding your PPE strategy?
Dr. Nanasy: Since a visit looks so much different for our established patients, we made a video that patients receive prior to their exam, detailing changes to protocols, equipment and experience. They not only know what to expect, but also are shown the efforts we are making for their safety.
Dr. Wilson: We posted signs at the entrance stating no entry without a mask. Our schedule has not changed, but we did put in place multiple new protocols and procedures for PPE, cleaning and safety.
Dr. Shida: We minimized the number of different rooms that a patient enters. We are looking at investing in some new equipment so that an exam room contains all equipment needed versus separate pre-testing/special testing rooms.
Current Challenges
Dr. Dillehay: Dr. Shida, I really like this idea of finding the ways to minimize “encounters” while patients are in the office. Can you or others share additional thoughts on this topic? What else is keeping each of you up at night?
Dr. Shida: Without a doubt, keeping staff healthy has been a challenge; even 1-2 days of a staff being out can impact any practice. The fogging of the phoropter lenses with patients wearing face masks has been very difficult to avoid. Once the phoropter lenses are fogged up, the refraction accuracy becomes compromised. A patient’s vision can suddenly decrease to 20/30-20/50 with fogging, and patients can lose confidence in the refraction.
Dr. Nanasy: We are looking for the “sweet spot” of having the most patient encounters possible, without becoming too busy juggling new procedures and extended wait times. We were wasting time dealing with the awkwardness of educating patients about keeping their masks on and dealing with the phoropter and glasses fogging, but have since found ways to overcome those obstacles.
Dr. Schornack: Minimizing potential changes in schedules, staffing and examination flow are critical to keep everyone moving. Clear and consistent safety protocols help minimize absences. People out for quarantine pending testing results can wreak havoc with scheduling and continuity of care.
PPE Costs
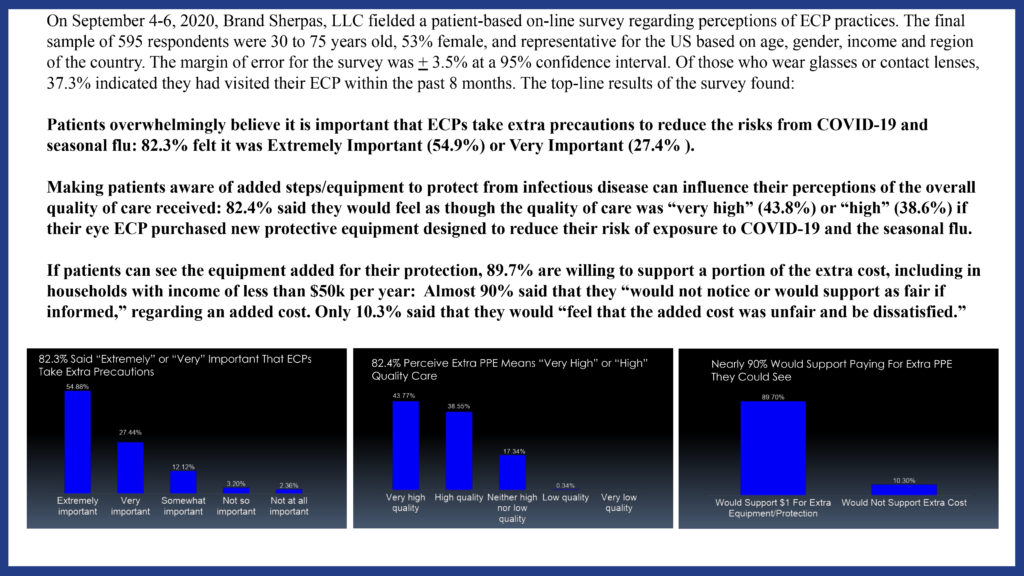
Dr. Dillehay: As each of you have shared, we are investing more time and resources in our practices during this crisis and for the foreseeable future. A recent survey of almost 600 patients overwhelmingly believed ECPs should take extra precautions to reduce the risks of contamination, and almost 90 percent of patients were willing to help cover the costs. What recommendation would you make to your colleagues, as Jobson found most ECPs (65 percent) are not passing on this cost?
Dr. Nanasy: We need to find ways to cover these increased costs. We are integrating retinal photos and OCT scans for every comprehensive exam. We are covering our PPE costs by the higher number of patients that now do the additional testing. We do need to cover our costs, and patients seem more open to a higher overall examination fee than paying for a separate PPE fee.
Dr. Wilson: At this point we have not yet increased fees, but this issue is something we need to evaluate further. One thing we are doing is more screening retinal images, and that helps to offset the increased costs of PPE and safety and cleaning protocols.
Dr. Shida: We have not added the cost to our patients, but recognize that it is an important decision for our practice. At the end of the year, we are planning to increase our fees across the board and add it in at that time.
Dr. Schornack: Most people underestimate the cost of the PPE in terms of just not the cost of the physical equipment, but inventory, and also staff ordering time. We need to evaluate it as part of the overall cost of providing services to patients.
PPE Innovation
Dr. Dillehay: As many of you have stated, it is critical for us to change and show up differently in order to best serve our patients, especially when it comes to incorporating new products and innovation into our practices. There is some new innovation launching this month, which was developed by an eyecare professional, Dr. Elvin Fenton, for eyecare professionals.
 The VisibleBliss Phoropter Mask is now available in the U.S., being launched exclusively by ABB Optical Group. It is a single use (disposable), non-gas permeable, breath shield for the phoropter. It would be great to get your insights on this innovation and your clinical experience with this product.
The VisibleBliss Phoropter Mask is now available in the U.S., being launched exclusively by ABB Optical Group. It is a single use (disposable), non-gas permeable, breath shield for the phoropter. It would be great to get your insights on this innovation and your clinical experience with this product.
Dr. Raynor: The VisibleBliss Phoropter Mask has been a godsend for reducing fogging of the phoropter lenses and examination efficiency. It provides an extra measure of safety and protection and allows for a fog-free refraction. Patients leave with the impression that we did everything possible to ensure their safety.
Dr. Nanasy: Patients are now coming with higher expectations regarding safety and office protocols. Patients have been impressed that we are using the disposable VisibleBliss Phoropter Mask for every exam. We make sure every patient sees us not only install it but then also toss it into the recycle bin. It often prompts patients to also discuss all our other safety protocols. It’s definitely leaving a lasting impression on our patients.
Dr. Wilson: Those patient sneezes, coughs, and breathing on the back of your hand (even with a mask) are virtually impossible to avoid. The VisibleBliss Phoropter Mask creates a much needed barrier, which allows me to focus on providing the highest quality of care. It also helps reduce lens fogging, which is a huge bonus. It really strikes you that the fogging is actually due to potentially contaminated breath droplets, which don’t come off quickly or easily. The amount of condensed aerosol breath that is captured by the single use VisibleBliss Phoropter Mask is astonishing, and that means it is not being spread toward me!
Dr. Shida: We tried everything to stop phoropter lens fogging. Patients had to sit back and wait 1-5 minutes for the lenses to clear up. Using a cotton tipped applicator to clean the lenses created a hassle, as the fog is very dense and concentrated. It just was not a smooth experience. Everyone would get frustrated, lose confidence in the refraction, and slow down the examination flow. I tell patients as I put the VisibleBliss Phoropter Mask on the phoropter, that it reduces the fogging of their vision and is designed to protect them from me and me from them. It increases patients’ confidence in the results and allows them to see the extra steps and precautions taken to ensure a safe and comfortable examination.
Dr. Schornack: Patients and staff appreciate taking every precaution possible to protect their health and safety. A disposable breath shield for the phoropter offers the advantage of minimizing the potential of touching a contaminated surface.
Dr. Dillehay: The VisibleBliss Phoropter Mask serves as a non-gas permeable barrier between the doctor and patient, and provides additional protection for both. The disposability helps to minimize staff contact with a potentially contaminated surface such as might occur with cleaning of a reusable breath shield.
Moving Forward
Little things like using the VisibleBliss Phoropter Mask on every exam can quickly become “big things” in the eyes of our patients. This pandemic has forever shaped people’s behaviors, and our patients will be evaluating us differently now and in the years to come.
We can learn from some of the most iconic brands in the world, as they quickly show us how important our current and future behaviors can affect our patients. Think about the establishments you now frequent during the pandemic – whether it’s Chick-Fil-A or Starbucks or your personal favorite, the brand has given you the confidence they are doing the little things to help provide you with a better experience. As the panel stated, the VisibleBliss Phoropter Mask will have this same type of impact of extending trust and provide that “wow experience” patients did not expect before entering the exam room.
Businesses that make it through these challenging times will be those that win customer trust when it comes to safety and health. While 2020 may not have started off as we planned, it offers an opportunity to accelerate changes in our practices and position them for future growth. How patients view health-care practitioners has forever changed; those practices that can adapt and emphasize health and safety will find the rewards will be to the overall health of their patients and their practices.
Editor’s Note: The VisibleBliss Phoropter Mask has not been FDA cleared or approved. The product has been authorized by FDA under an EUA for use as source control by the general public as well as by Health Care Practitioners in healthcare settings as to help prevent the spread of infection or illness during the COVID-19 pandemic. This product is authorized only for the duration of the declaration that circumstances exist justifying the authorization of the emergency use of medical devices, including alternative products used as medical devices, during the COVID-19 outbreak, under section 564(b)(1) of the Act, 21 U.S.C. § 360bbb-3(b)(1) unless the authorization is terminated or revoked sooner. For further information, please visit https://abboptical.com/visiblebliss-phoropter-mask