Sponsored Content

By John Rumpakis, OD, MBA
Sept. 2, 2020
We are in interesting times. With the COVID-19 pandemic now into its seventh month, the “new normal” is starting to set in as we become adjusted to our modified clinical practices. With most practices operating at pre-COVID levels with respect to both patient volume and income, it has forced the practitioner to scrutinize and re-evaluate the services that they are providing. Lower-paying managed vision care examinations may have been acceptable in the old economy, but many are now revisiting whether or not they should accept a reimbursement that now barely covers the overhead on an hourly basis with the reduced patient volumes.
For practices that have embraced providing full-scope care, and having a mix of routine vision and medical eyecare that exceeds the national average of 80/20 range respectively and more in the 50/50 range, they are doing well. And those medical-based practices that are specializing in dry eye services are not just surviving, they are thriving.
Point-of-Care Gateway
We know that dry eye is one of the most prevalent conditions that affect the population. Whether your number is 15 percent of the population or 65 percent of the population that suffers from signs and symptoms of this disease, it is significant. Now if you are saying to yourself “My practice isn’t seeing those kind of numbers of dry eye patients,” then read on. I find that the key to a successful dry eye practice is being able to properly identify those individuals with signs and symptoms of dry eye early in the disease process. The problem is that we don’t ask any questions because the patient doesn’t mention it, and the patient doesn’t proactively ask because we are not asking the right questions; the proverbial chicken and egg dilemma. Fortunately this is an easy process to change.
Every patient should be provided with a qualified questionnaire about dry eye. Pick your favorite whether it is the Standard Patient Evaluation of Eye Dryness (SPEED), OSDI, DEQ5 or any of the others that are out there. Make this a mandatory part of your practice paperwork that a patient is required to complete. If a patient has a positive sign or symptom related to the questionnaire, then have a standing order for point-of-care testing to be done for both inflammation and osmolarity, optometry’s new vital signs as they are called. In doing this one simple step, you are widening the top of the funnel and capturing those patients who are symptomatic of dry eye, and by performing the point-of-care testing as a standing order you are now fulfilling one of the components of medical necessity for further dry eye evaluation.
It has been nearly six years since the InflammaDry test was approved for detecting elevated levels of matrix metalloproteinase 9, a clinically relevant inflammatory marker, in the tears of patients with dry eye disease. If you don’t know, InflammaDry is a single-use test that requires no additional equipment to administer or interpret results. It takes less than two minutes to complete and results are available in 10 minutes, allowing a treatment plan to be established with the patient during his initial office visit.
The CPT code for InflammaDry is 83516 and is defined as follows:
“immunoassay for analyte other than infectious agent antibody or infectious agent antigen; qualitative or semiquantitative, multiple step method”
It is a CLIA waived test that can be performed in optometrists’ offices where the practice has a clinical lab designation and a physician with the practice has been registered as a clinical lab director. It is a tech-administered test, and the current national payment amount for this lab test is $11.53 per eye. CLIA waived point-of-care tests are generally not subject to co-pays or deductibles, and should be billed with the QW modifier. Some commercial carriers may not require the QW modifier.
One of the most important aspects about these tests is the ability to have a standing order for them to be performed if the patient presents with a sign or symptom from a qualified questionnaire. And if you are following my recommendation about having every patient, on every visit fill out the questionnaire, you will find that you have many more dry eye patients in your practice than you thought.
Economic Impact
Optometry is in a unique place within the greater health-care framework. We have the largest labor force, and provide the vast majority of primary vision care to the 330 million U.S. population. Yet, to a large extent, we don’t recognize the potential impact that we can have on patient care because sometimes we are either just “too busy,” or not aware of our capabilities, and our patient’s acceptance of those capabilities, to realize what we can truly do to improve patient care in the area of dry eye.
The economic impact of doing consistent, sign- or symptom-driven point-of-care testing can be profound, particularly in the COVID economy. Moreover, it provides you with the starting point for a conversation with the patient about their symptoms, and the results of their test. As stated earlier, a positive sign or symptom, followed with a positive result from your InflammaDry test is all you need to start thinking about performing a dry eye workup on your patient.
So now let’s focus on the profitability of being proactive in identifying, diagnosing and treating dry eye. Again, I am going to be extremely conservative in my calculations.
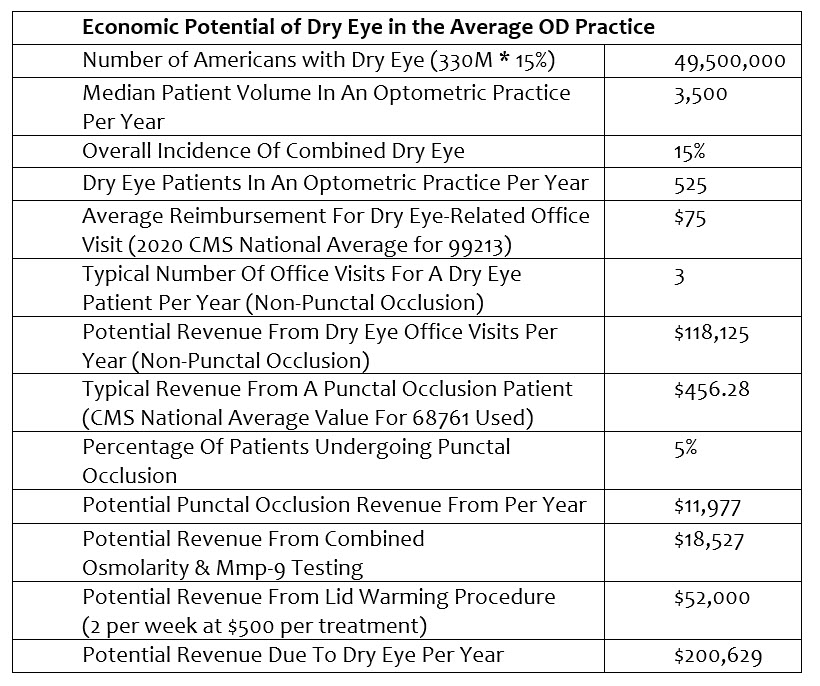
Please note, I didn’t calculate any photography, meibography, lid debridement, intense pulsed light (IPL), neutraceutical recommendations, or long-term (multi-year) income etc… into my calculations as I wanted to be extremely conservative in my approach. I also used National Average values for procedures based upon the 2020 CMS fee schedule, knowing that while they are significantly below market rate, they are public data for reference purposes.
So why is $200,629 a significant figure? The average income for an optometrist in the U.S. today is well below $200,000, and the median income is less than the average. If you can add a single sub-specialty that has built in demand, known incidence and prevalence, doesn’t require a heavy front-end investment to incorporate, and deliver high levels of patient satisfaction, reduce your optical redo rate, and can provide a 100 percent increase in income, then I would say it becomes something very attractive to consider incorporating into your practice.
Do It Now
Incorporating a qualified questionnaire and standing orders for point-of-care testing such as InflammaDry into your daily practice routine can have profound effects on your patients and your practice. Widening the top of the funnel and eliminating the “chicken and egg” problem means that you are doing your best in properly identifying your patients, getting vital clinical data, and having the ability to bring them the very best in clinical care to help them manage this potentially debilitating disease and improve their quality of life.
 John Rumpakis, OD, MBA, is Founder & Chief “Make It Happen” Officer of Practice Resource Management, Inc. To contact him: John@PRMI.com
John Rumpakis, OD, MBA, is Founder & Chief “Make It Happen” Officer of Practice Resource Management, Inc. To contact him: John@PRMI.com





















