By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

Oct. 7, 2020
Every practice is going to experience third-party claim denials. Some denials are fixable, such as claim submission problems (incorrect or incomplete information) or third-party processing errors, and some are not fixable, such as lack of coverage issues. Sometimes fixes are easy to make and other times the fixes take additional work. No matter the reason, every practice should have a process for handling the denials. These three steps will give you a starting place for that process.
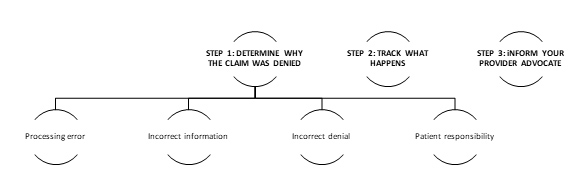
STEP 1: DETERMINE WHY THE CLAIM WAS DENIED AND FIX IT
You can find this answer on the explanation of benefits (EOB) forms and/or Remittance Advice (RA) you receive from third parties. Third party/insurance carriers use different denial codes indicating their reason(s) for nonpayment or why a claim was paid different than billed. The Claim Adjustment Reason Codes (CARCs) communicate why you were paid differently than billed. Two examples would be: (1) patient responsibility and (2) charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement.
If you were paid differently than billed, and there is no CARC on the claim payment line, you should contact the carrier to find out why.
PROCESSING ERROR
Often, if the problem is a processing error, a simple call to the carrier may resolve the issue.
Two words of advice – be kind. It is not helpful to take your anger out on the person at the third party answering the phone. The old adage that you get more with honey than vinegar is always true when dealing with third parties.
If this does not resolve your denial, then you need to follow the Incorrect Denial suggestions.
INCORRECT INFORMATION
When the claim is denied due to incorrect information, make corrections and resubmit the claim to the carrier using their corrected claims process.
INCORRECT DENIAL
If the claim should have been paid, yet the carrier as incorrectly denied the claim, then you will need to submit an appeal/reconsideration. Not every carrier has the same process, so you will need to follow the carrier specific appeals process. This process can usually be found on the carrier web site.
PATIENT RESPONSIBILITY
When there is a lack of coverage, or there is a fee schedule/maximum allowable or contracted/legislated fee arrangement, the patient is often responsible to pay the bill. Be careful to follow balance billing rules and Advance Beneficiary Notice of Noncoverage (ABN) rules.
STEP 2: TRACK WHAT HAPPENS
You must be organized to track the denials and what happens so that you can follow up on any claim very easily. Create two folders in your computer: open claims and closed claims. The open claims have not yet come to the end of the road. They are still in process of being resolved. File these by patient name, third party carrier and date of original claim so that you can sort them in each of these ways. Attach notes to the files make sure to keep track of who you contacted at the carrier, the date of contact and a short description of what was said or done. This will save you time in the long run and help get you to a fix faster.
Closed claims have been resolved.
STEP 3: INFORM YOUR PROVIDER ADVOCATE
Often denial trends occur with carriers. Sometimes it’s our fault, so that means we have an internal systems problem that needs to be resolved to fix the problem. More often, it is a carrier problem. When a high number of problem denials seems to be coming from a carrier, use this approach to fix the problem.
Other Articles to Explore
1. Contact Provider Relations at the carrier and ask to speak to a supervisor. (The people answering the phone do not have the ability to institute changes within the company, so you need to talk to someone who can actually fix the problem.) Explain the problem you discovered and make sure to have the claims ready to give specific examples to the supervisor so they can see the same problem you see.
2. When dealing with trend problems, contact your state optometric association chair of the third-party committee (or equivalent) and, if the carrier is a national carrier, also contact the AOA, so that both the state and national associations are aware of the problem and what you are trying to do to correct the situation. Be careful to follow HIPAA guidelines during this sub-step.
Claim denials take time – staff time and sometimes doctor time. There are only a finite number of hours in any day, so any time spent on dealing with claim denials is taking staff and doctors away from providing patient care. By having a defined process for handling claim denials, your goal is to get better and better at submitting claims and, therefore, spend less and less time dealing with claim denials.



























