By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD
Jan. 8, 2020
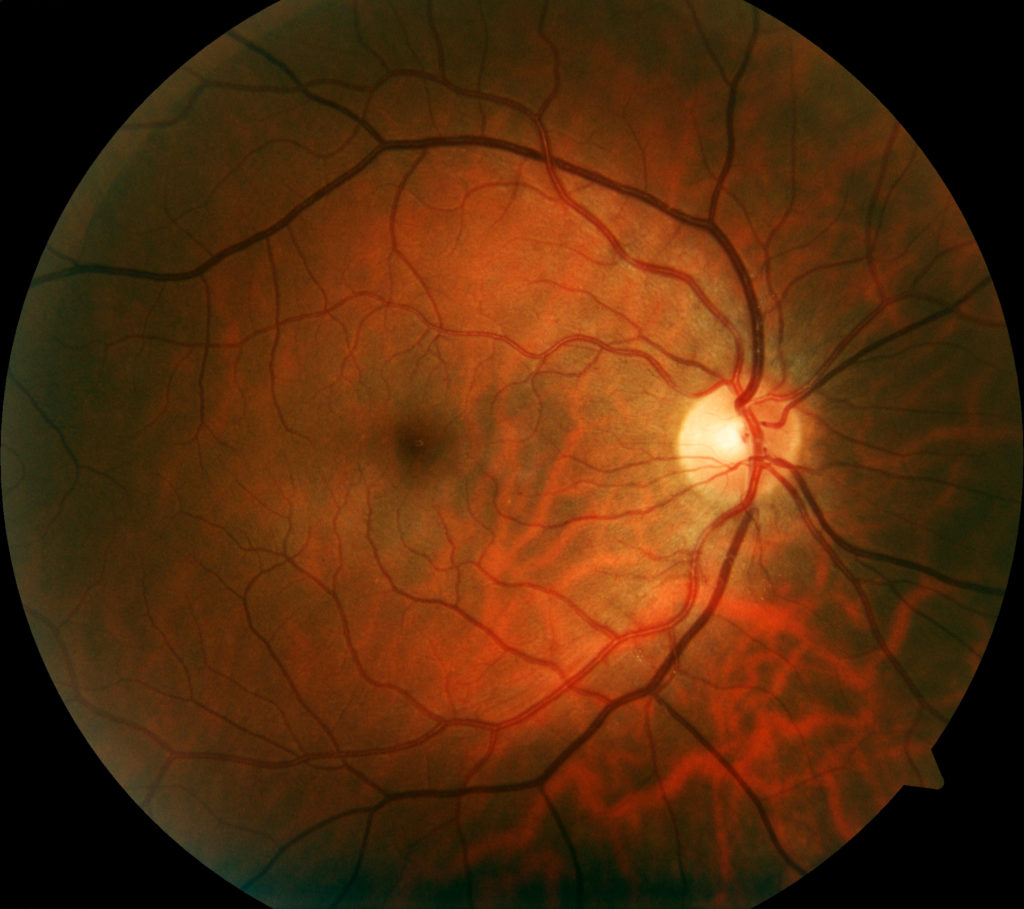
Extended ophthalmoscopy is a valuable tool in the diagnosis and treatment of patients, helping you to determine how you can best help them. Two changes take effect this year impacting how you code this procedure for reimbursement. Here are the details.
Every year codes change. It is important to keep up with the changes. This year was no different. One of the code sets that changed was Extended Ophthalmoscopy (EO). The previous CPT codes used for EO have been retired. The previous codes were: 92225 (Initial EO) and 92226 (Subsequent EO). The new codes are 92201 and 92202. Here’s the description for each of the two new codes.
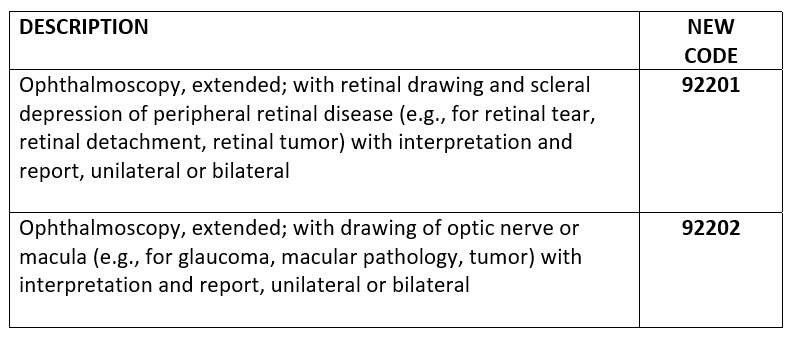
The change is from the retired codes which were for an initial and a subsequent EO to the new codes which are for EO targeting peripheral and central retinal problems.
Notice especially the description of the new code 92201. For 92201, the very important word “and” is placed into the description – “… and scleral depression …” If we are just talking about the procedure EO and its clinical use, scleral depression is not necessary every time you would use this procedure, however, does inclusion of the word “and” into the description for 92201 introduce the situation where an auditor would claim that scleral depression must be done every time the code 92201 is billed? The way the code is written, the answer is yes.
With its new definition, the AMA is redefining peripheral EO to only be paid if scleral depression is done. This has the impact of making eye doctors give up being paid for peripheral EO for those cases when scleral depression is not necessary. That’s a shame. This definition needs revisited.
The documentation requirements for EO include:
- A statement of medical necessity for the procedure.
- A medical order for the procedure.
- Documentation of the diagnostic technique used (e.g.: 90 D lens, scleral depression).
- A drawing that is clearly labeled representing the retinal pathology identified. Be sure to follow carrier documentation rules exactly.
- Interpretation and report that describes findings and includes an action plan.
Other Articles to Explore
Billing requirements include:
• You must have an abnormality in order to bill EO. Then, on subsequent visits, you need to have a change in the abnormality in order to bill EO again.
• For the new codes you get paid the same if you do one eye or both eyes.
• Fundus photography (92250) will not be separately billable the same day.
• Do not bill 92202 with 92201 on the same day.
• The new EO codes are bundled with all retinal minor and major surgeries.
Your action plan should be:
• Eliminate 92225 and 92226 from your coding going forward.
• Add 92201 and 92202 to your coding going forward.
• Make sure you follow the documentation requirements.
• Make sure you follow the billing requirements.
If you’d like to read more…
https://www.aao.org/practice-management/news-detail/billing-ophthalmoscopy-testing
https://help.eyefinity.com/regulatory/CPT/2020/New_CPT_Codes_Effecti.htm#Extended
https://www.retinalphysician.com/newsletter/practice-management-insider/november-2019
https://www.3mhisinsideangle.com/blog-post/a-look-ahead-to-the-2020-cpt-changes/

























