By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

Dec. 9, 2020
COVID-19 is still rampaging through the country, and putting stress on businesses, including eyecare practices. Here is what the latest findings of Jobson Optical Research’s COVID-19 ECP Impact Survey reveal, and how you should respond in your practice.
 Ninety-seven percent of practices in the country are open. Of the 3 percent of practices that are not open, there has been a slight uptick of 6 percent from the last survey (from 46-52 percent) of practices planning to reopen. That is a good trend.
Ninety-seven percent of practices in the country are open. Of the 3 percent of practices that are not open, there has been a slight uptick of 6 percent from the last survey (from 46-52 percent) of practices planning to reopen. That is a good trend.

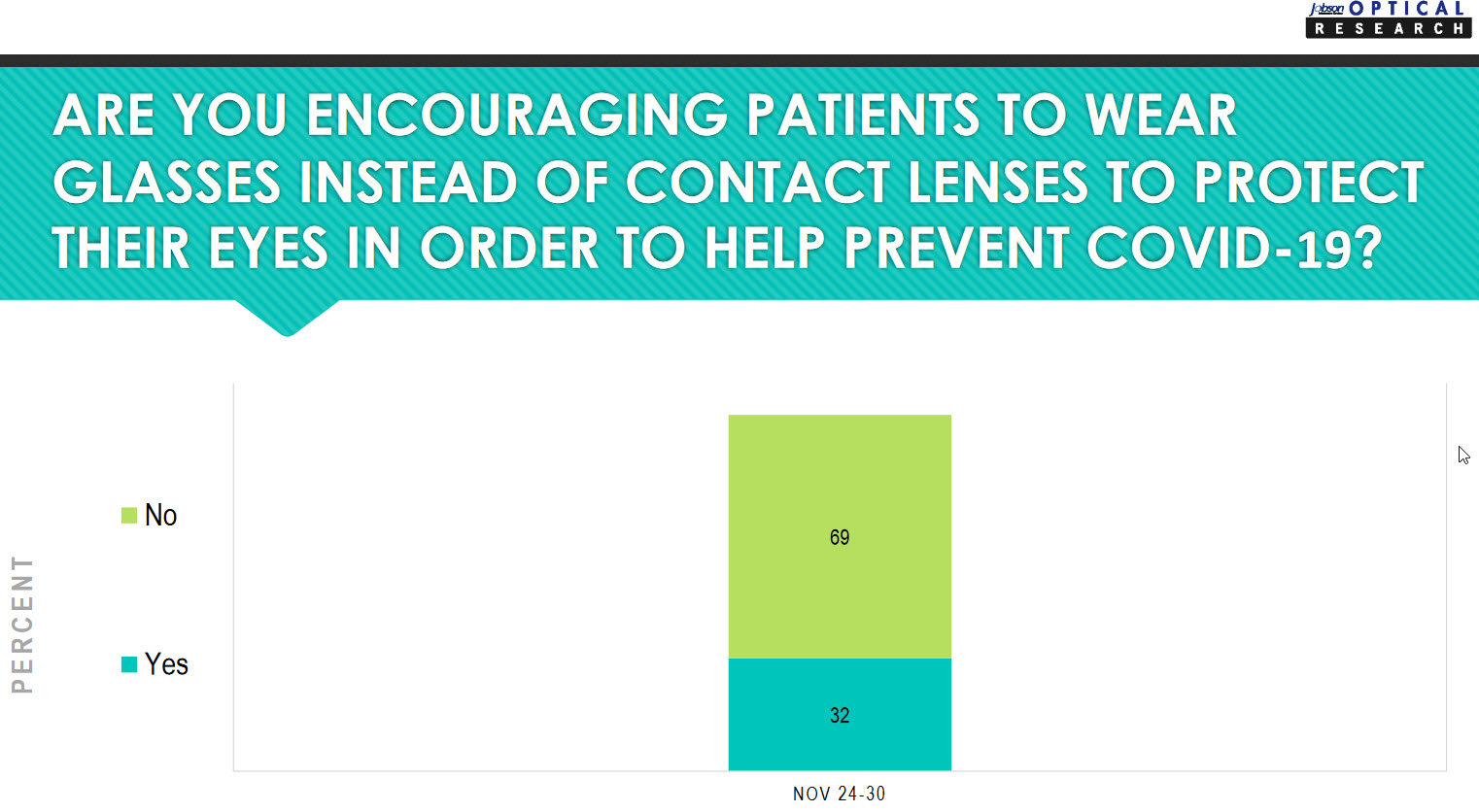
Thirty-two percent of practices are encouraging patients to wear glasses instead of contact lenses to help prevent a COVID-19 infection. Over two-thirds of practices are not taking this action.
The thinking behind moving from contacts to glasses is: “SARS-CoV-2 RNA has been found in tears of the infected patients, and reports suggest that the ocular surface could serve as a portal of entry and a reservoir for viral transmission.” Excellent hygiene including hand washing and not touching the eyes will need to be emphasized to patients wearing contact lenses.
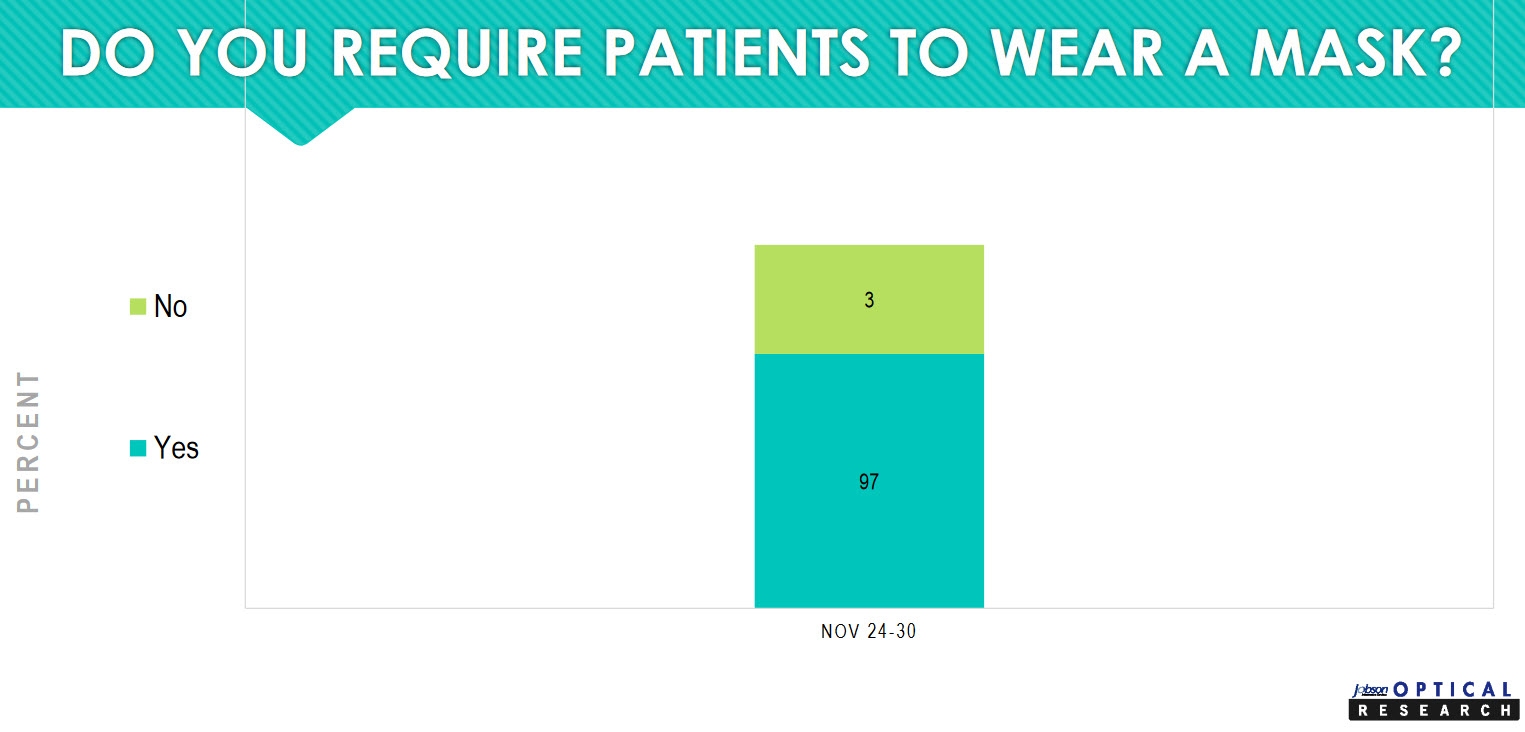
At 97 percent, the overwhelming majority of practices are requiring patients to wear a mask.
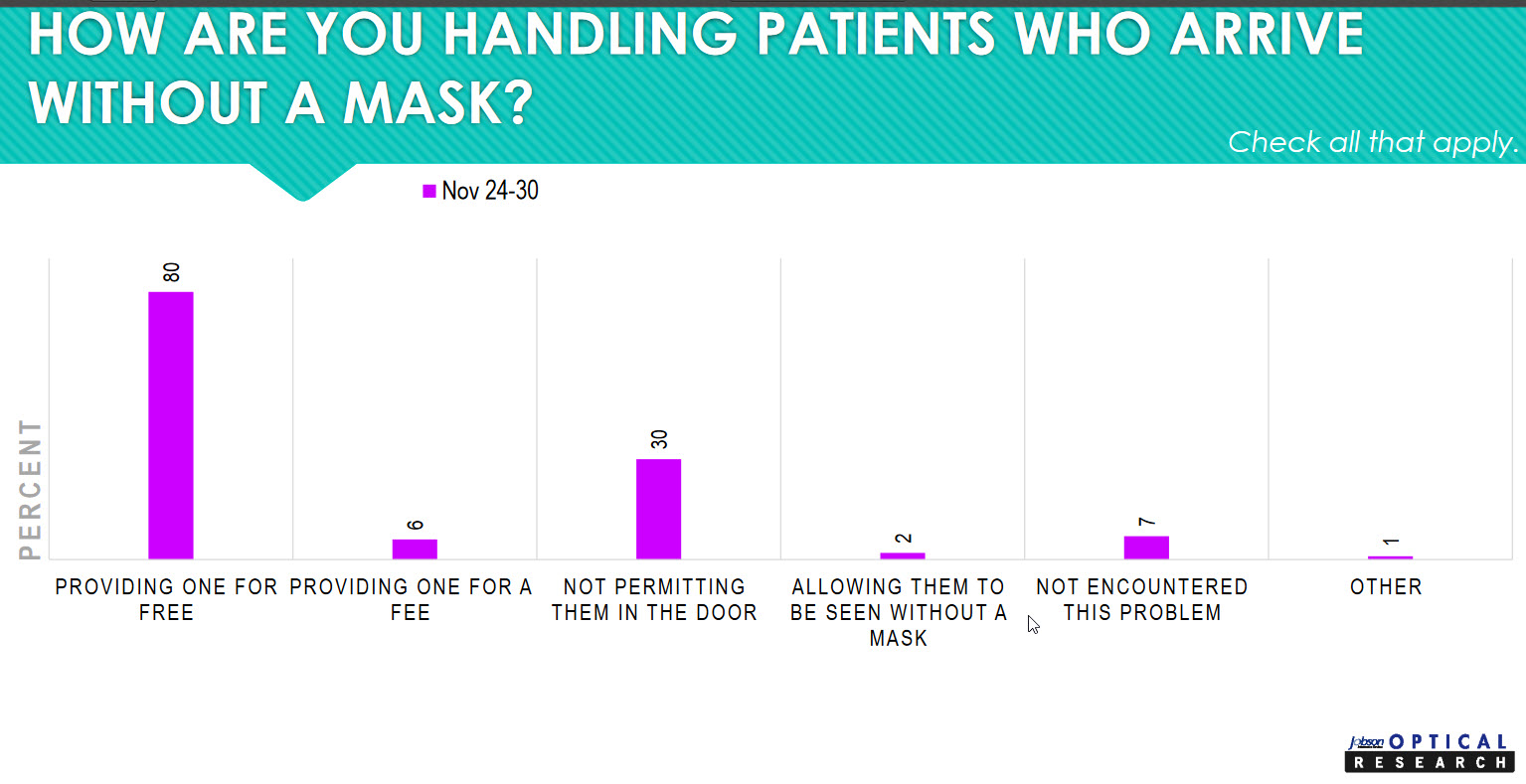
The interesting question is how practices are handling those patients who arrive without a mask. Most practices (80 percent), are providing a mask for free. Six percent are providing one for a fee. Thirty percent of practices are not permitting a patient who is refusing to wear a mask in the door. This follows the “I wear my mask for you, and you wear your mask for me” philosophy. If a patient is unwilling to wear a mask to keep the other patients in the office, my staff, and me, safe, then it seems reasonable not to allow them in.
One of the principal precepts of bioethics is to “do no harm.” All health-care personnel are taught to consider the possible harm any action or inaction might do. It’s good to see that this principle is being followed in eyecare practices.
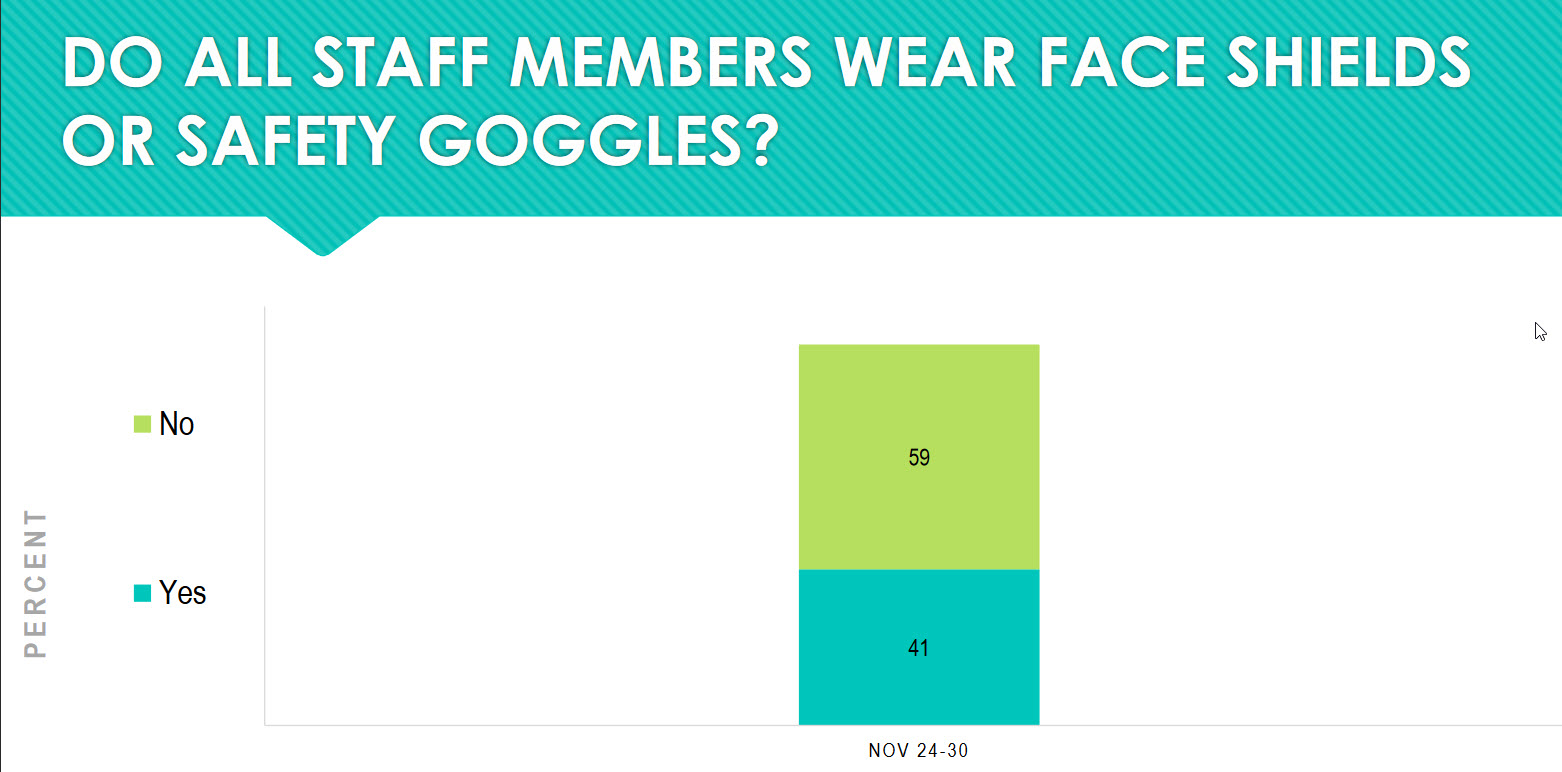
In some practices (41 percent), staff members are going the extra step of wearing face shields or safety goggles. No studies we are aware of show that this extra step is necessary in practices that do not have patient fluids being stirred up, such as occurs in dental practices or surgical suites. If this extra step helps staff and patients to feel safer, that is fine because no harm is being done. The exception in an eyecare practice, when a face shield or safety goggles would be needed, is when a corneal foreign body is being removed.
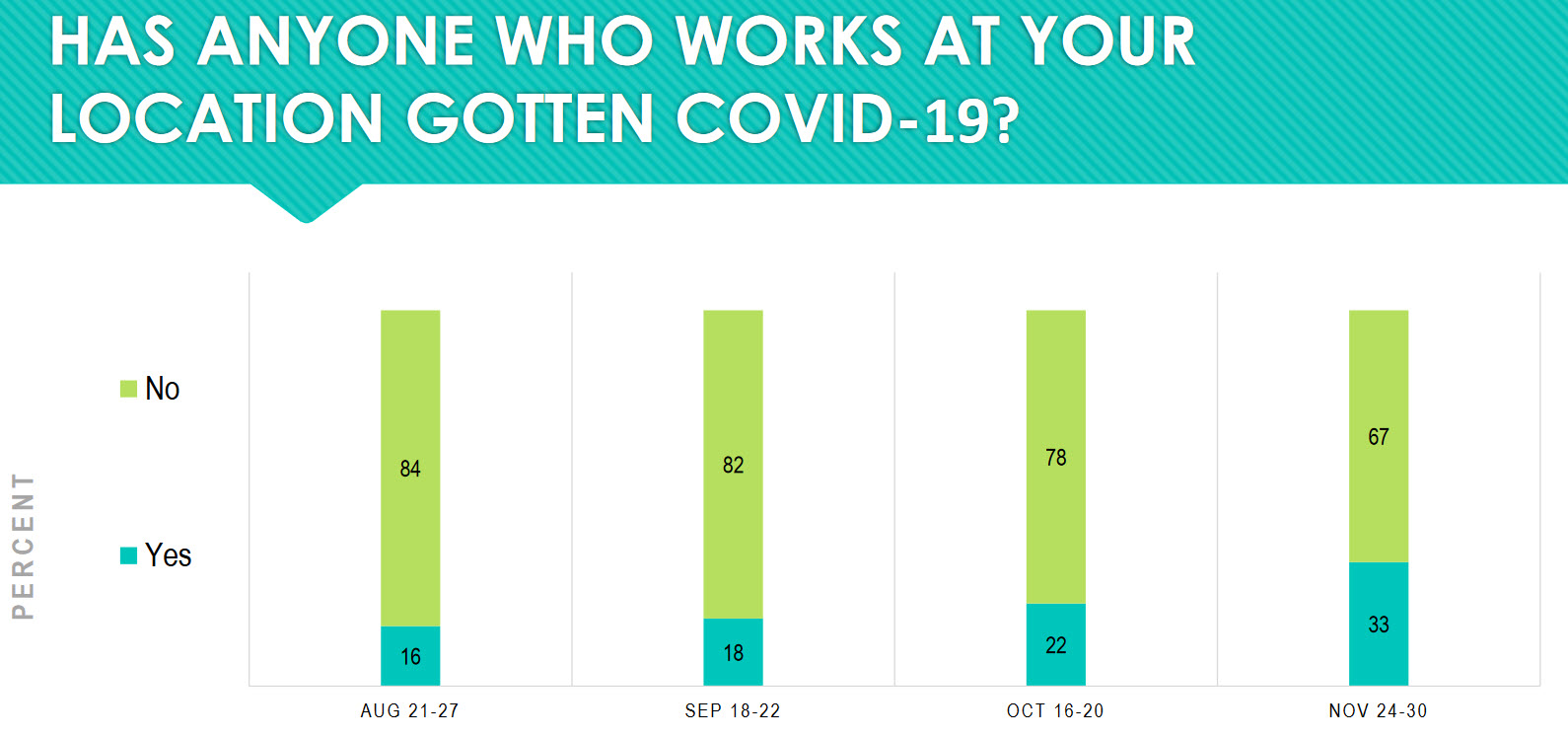
Thirty-three percent of practices report someone who works in the practice has gotten COVID-19. That’s up from 22 percent roughly a month prior. That’s to be expected. The longer the pandemic goes on, the more people we should expect to be infected. The practical result of this is that the practice must have in place the following four protocols:
1) What to do if someone is infected or has come in contact with someone who is infected.
2) What to do for staff members or patients who interacted with the infected or exposed staff member.
3) Decide how long must the infected or exposed staff member self-isolate
4) Decide what steps must occur before the staff member can return to the office.
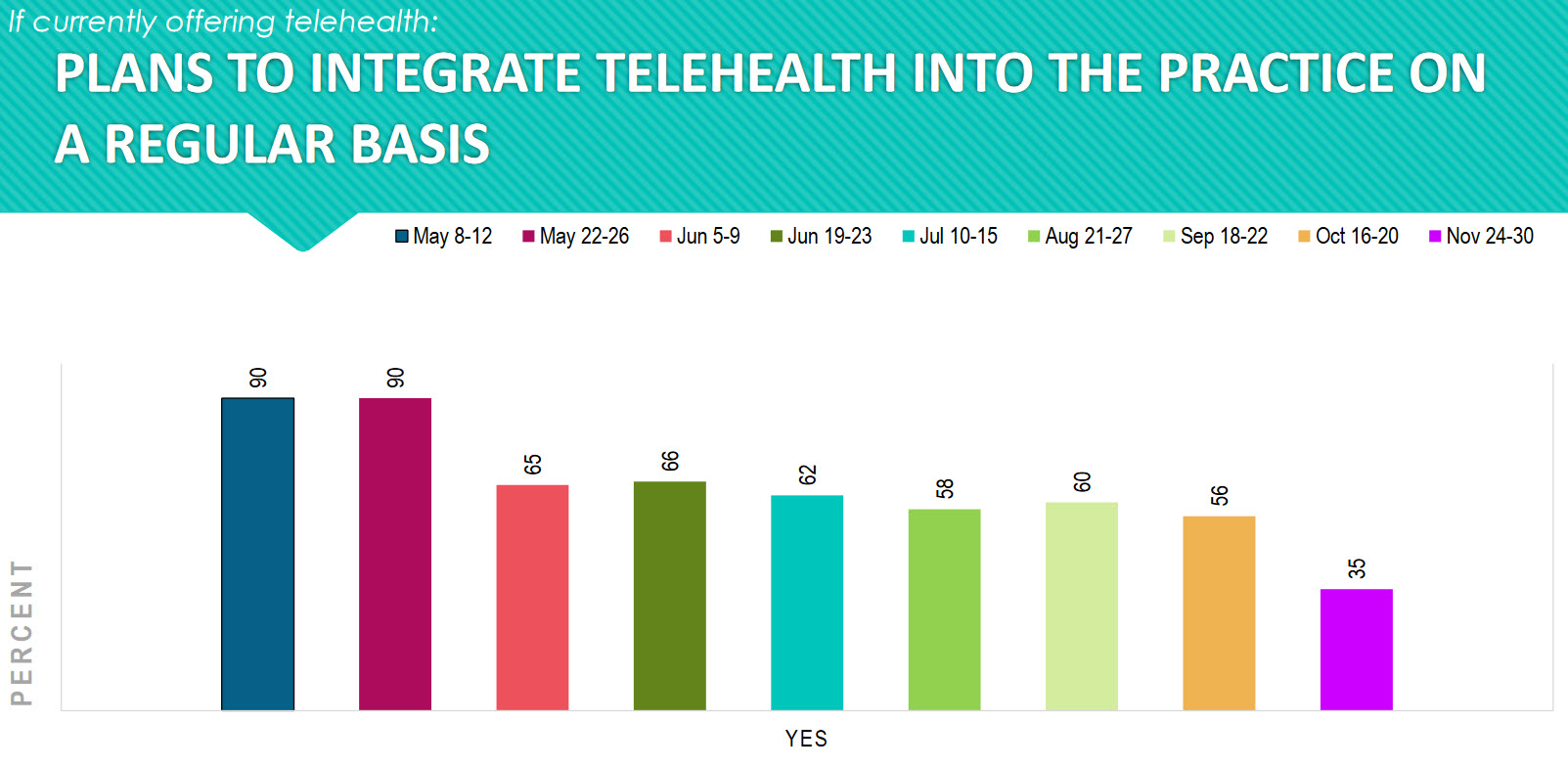
As practices have opened back up, the interest in telemedicine has decreased from a high of 90 percent in May to a low of 35 percent in November. We should keep our eye on this trend because the rest of the health-care world is moving toward a strong interest in telemedicine. There are opportunities here that may be missed if we just go back to business as usual.
We found it interesting to see the spread from 15 minutes to two hours per day of cleaning the office and exam rooms. There is clearly a balance to be had between efficiency and effectiveness. Maybe another way to ask this question is, “How much time per patient is spent disinfecting areas touched by patients?” If you are adding 30 seconds per “stop” (i.e.: reception/front desk, pretest, exam, optical, checkout) then that would be 2.5 minutes per patient of cleaning. If you are seeing 20 patients per day per doctor, then you are adding 50 minutes to your day per doctor just cleaning. The question then becomes, do you extend your day 50 minutes or do you decrease the number of patients seen? Or, the obvious question, do you become more efficient?

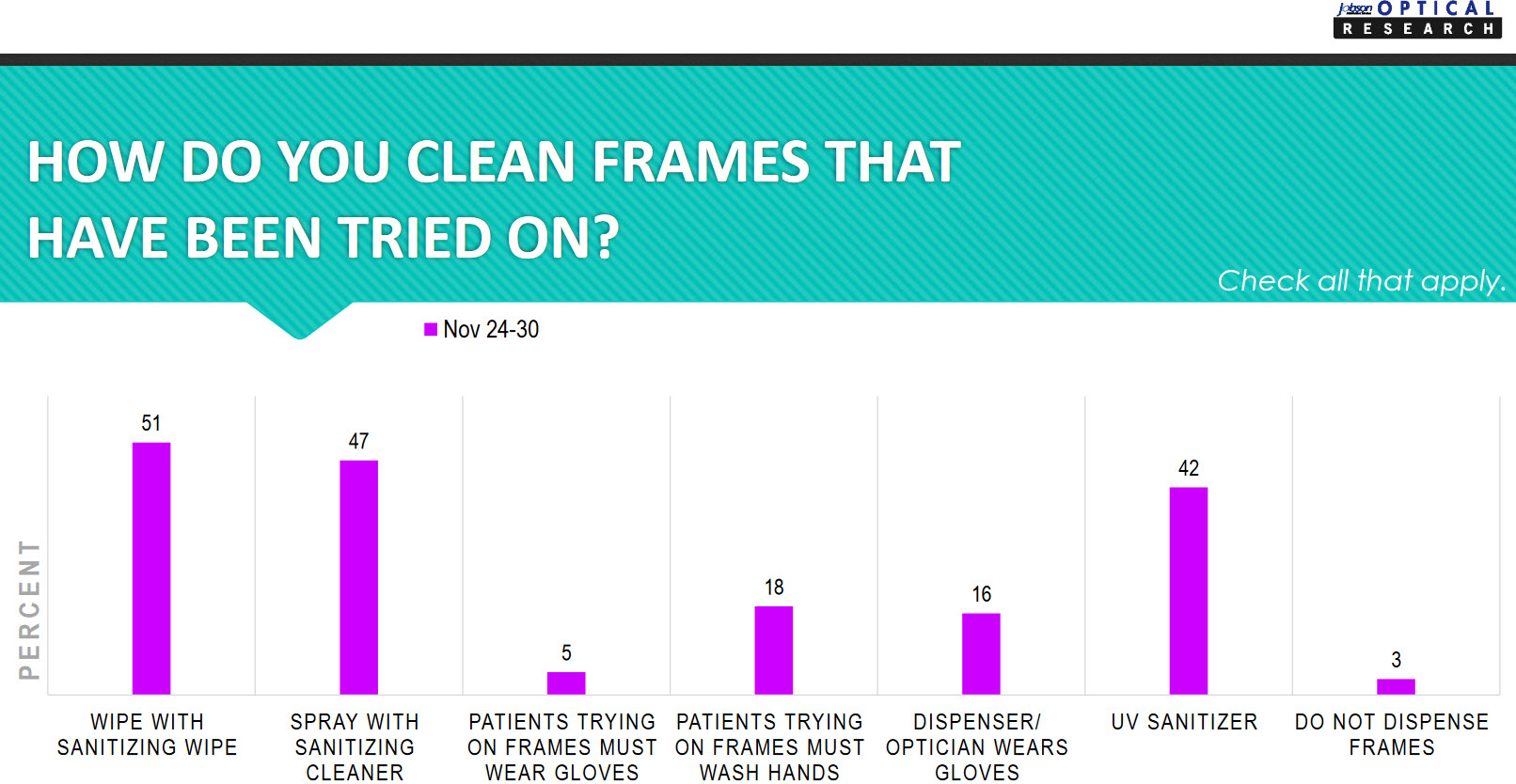
It is interesting to see the variety of answers to how frames that have been tried on are cleaned in offices. The ultimate focus here is to keep patients and staff safe no matter what methods are being used.
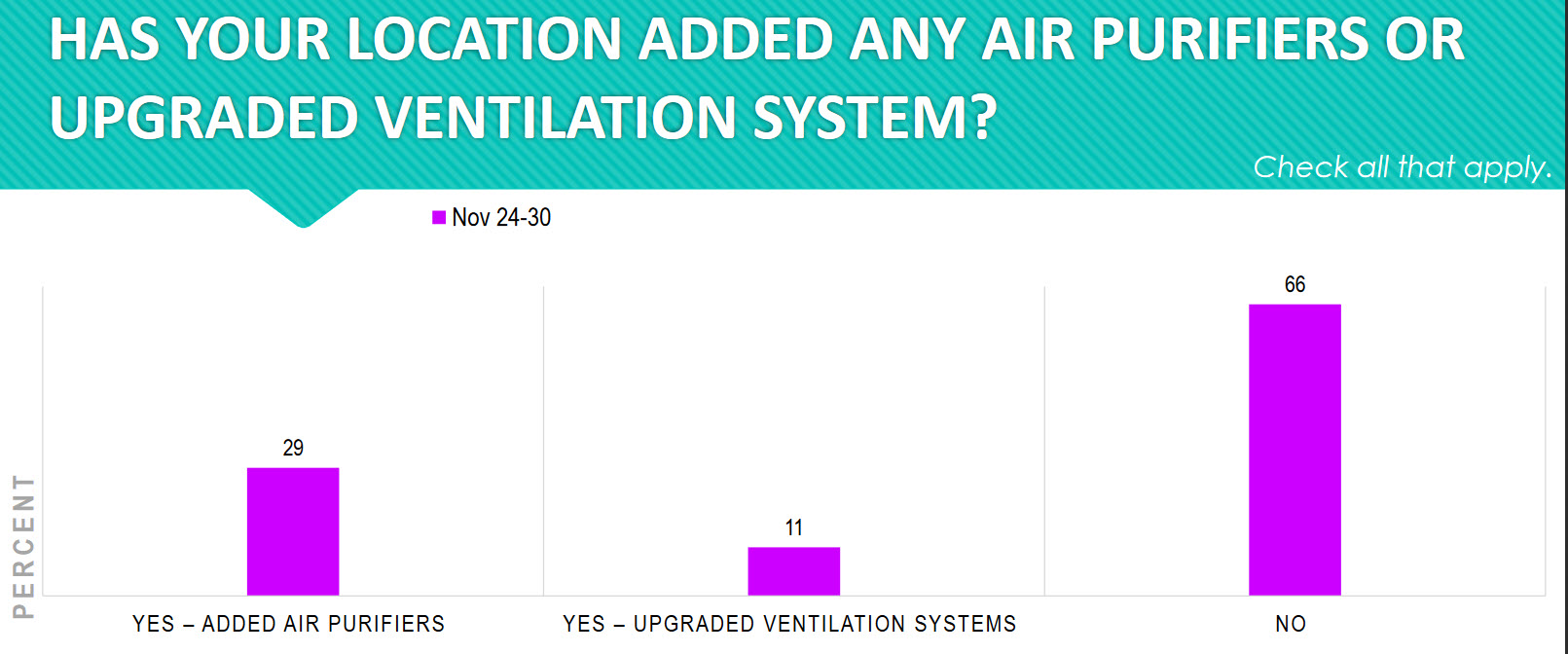
Forty percent of practices (29 percent + 11 percent) either added air purifiers or upgraded their ventilation systems. This is another step practices have taken to reduce exposure and help keep patients and staff healthy.
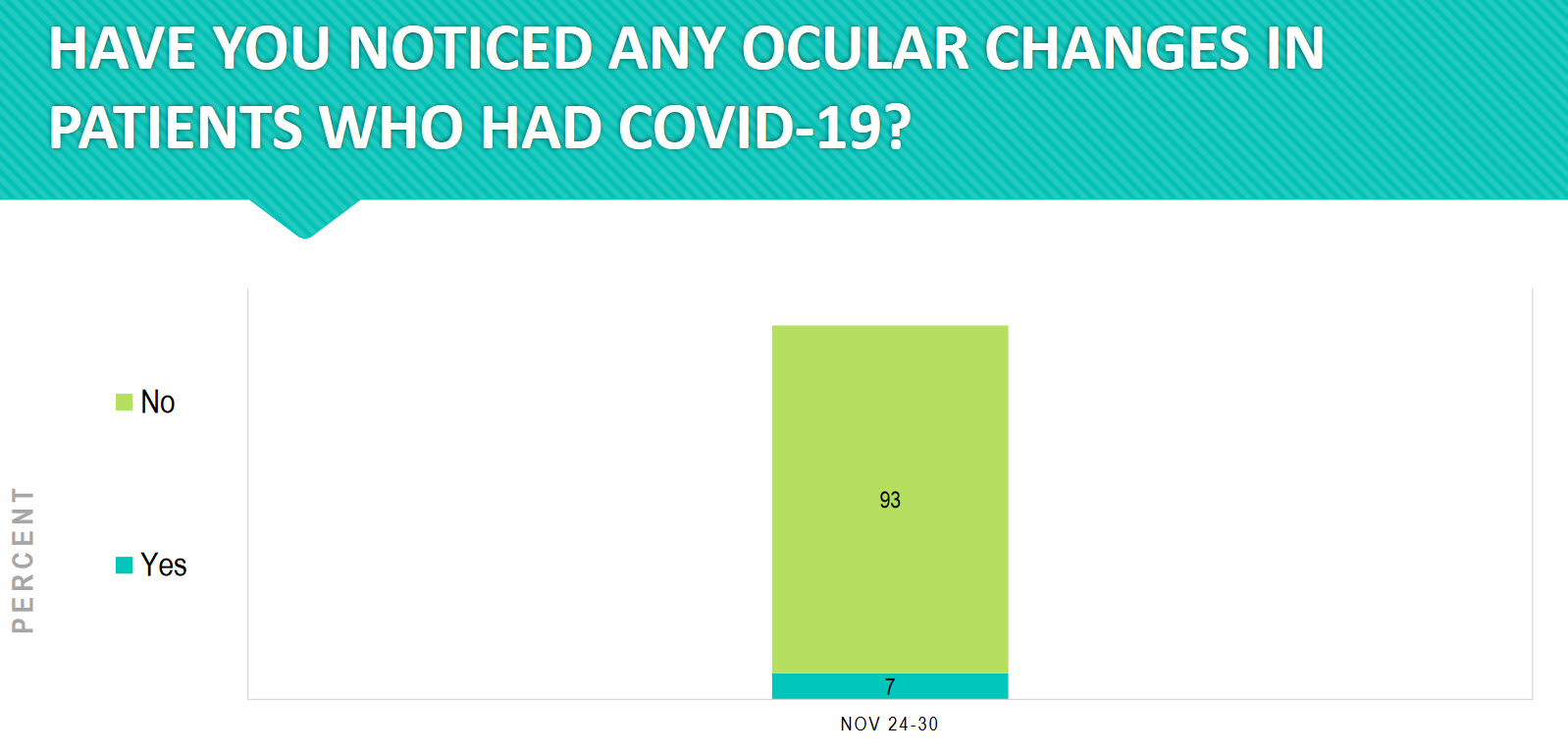
Ninety-three percent of practices have noticed ocular changes in patients who had COVID-19. This is an area that we need to follow closely going forward.
“Subtle retinal changes like hyperreflective lesions in the inner layers on optical coherence tomography (OCT), cotton-wool spots, and microhemorrhages have also been reported. In addition, COVID-19 has been associated with an increased incidence of systemic diseases like diabetes mellitus and Kawasaki disease, which are particularly relevant for ophthalmologists due to their potentially severe ocular manifestations.” i
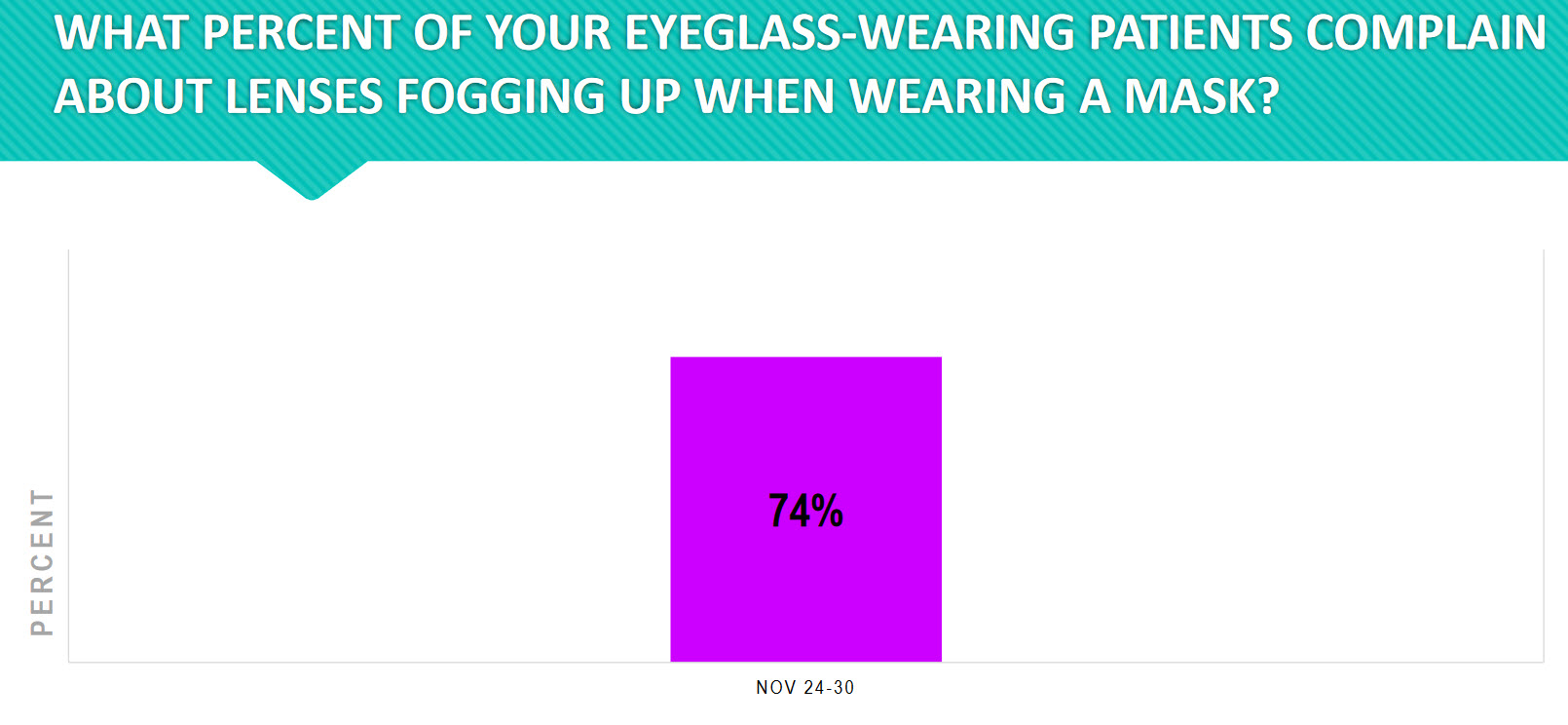
Lens fogging is a common complaint among mask wearers. Every excellent practice has already identified this problem and is offering patients effective solutions. What solutions are you offering your patients?
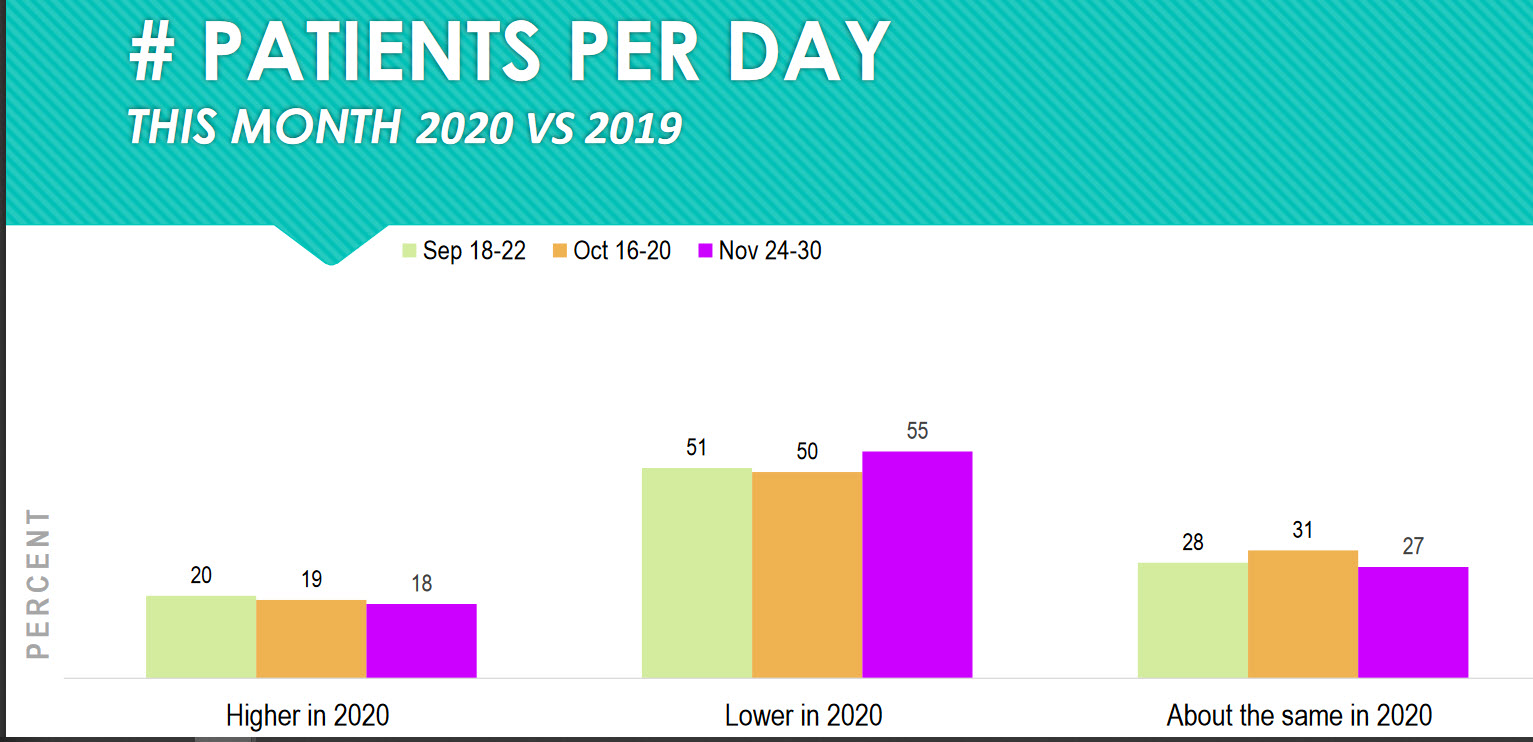
Forty-five percent of practices are seeing the same or higher numbers of patients this month versus the same month last year. That is excellent! It means that practices are finding ways to be both efficient and effective in seeing patients. The other 55 percent of practices need to re-evaluate patient flow and procedures to improve their performance.
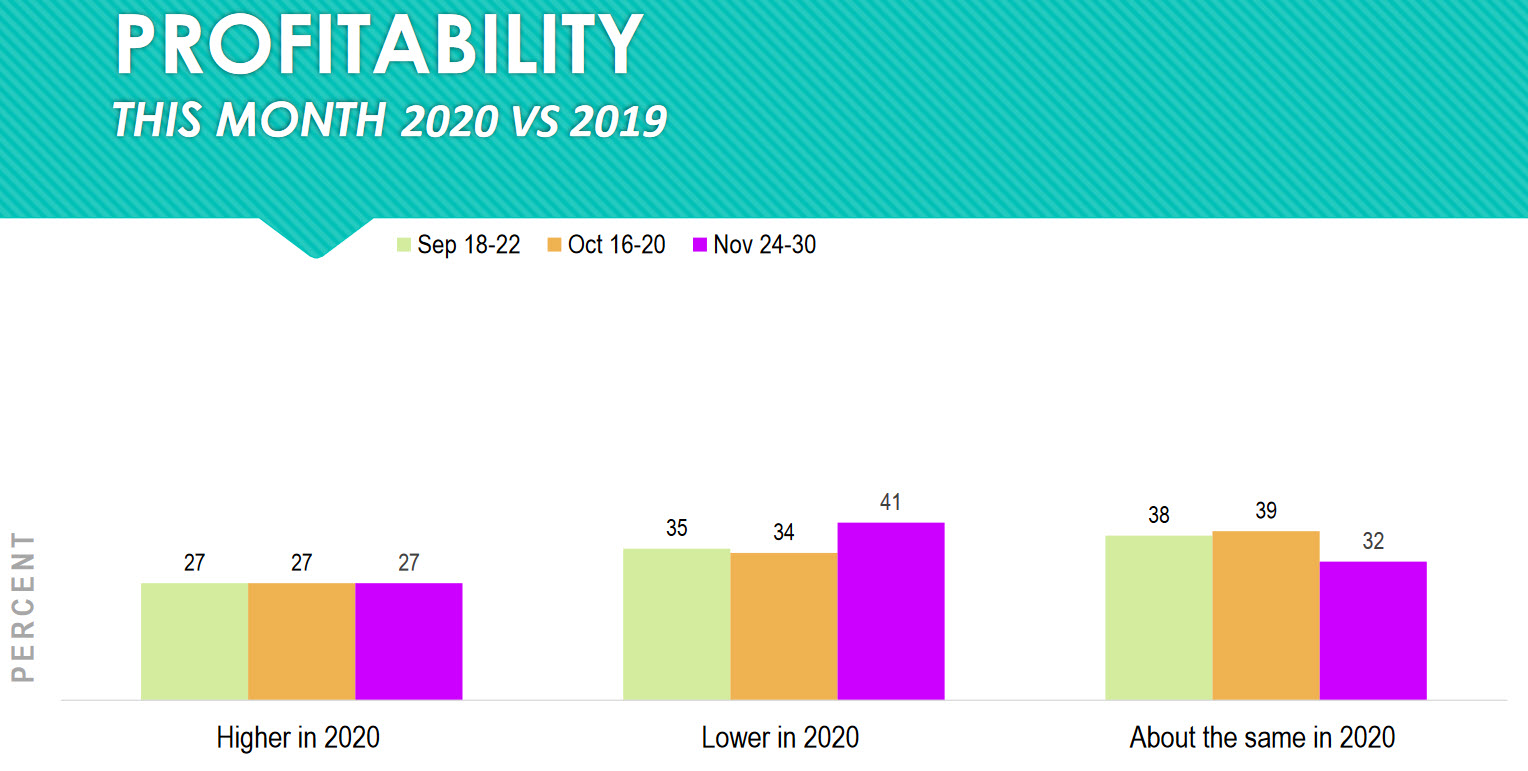
Fifty-nine percent (32 percent + 27 percent) of practices are reporting they are as profitable, or more so, in November this year compared to November last year.
A business that is not profitable will soon be out of business. Any eyecare practice that is out of business cannot provide care to anyone. A profitable practice has the resources to purchase better equipment, hire more staff, expand office hours. A non-profitable practice can do none of those things, so it is essential that a practice is profitable.
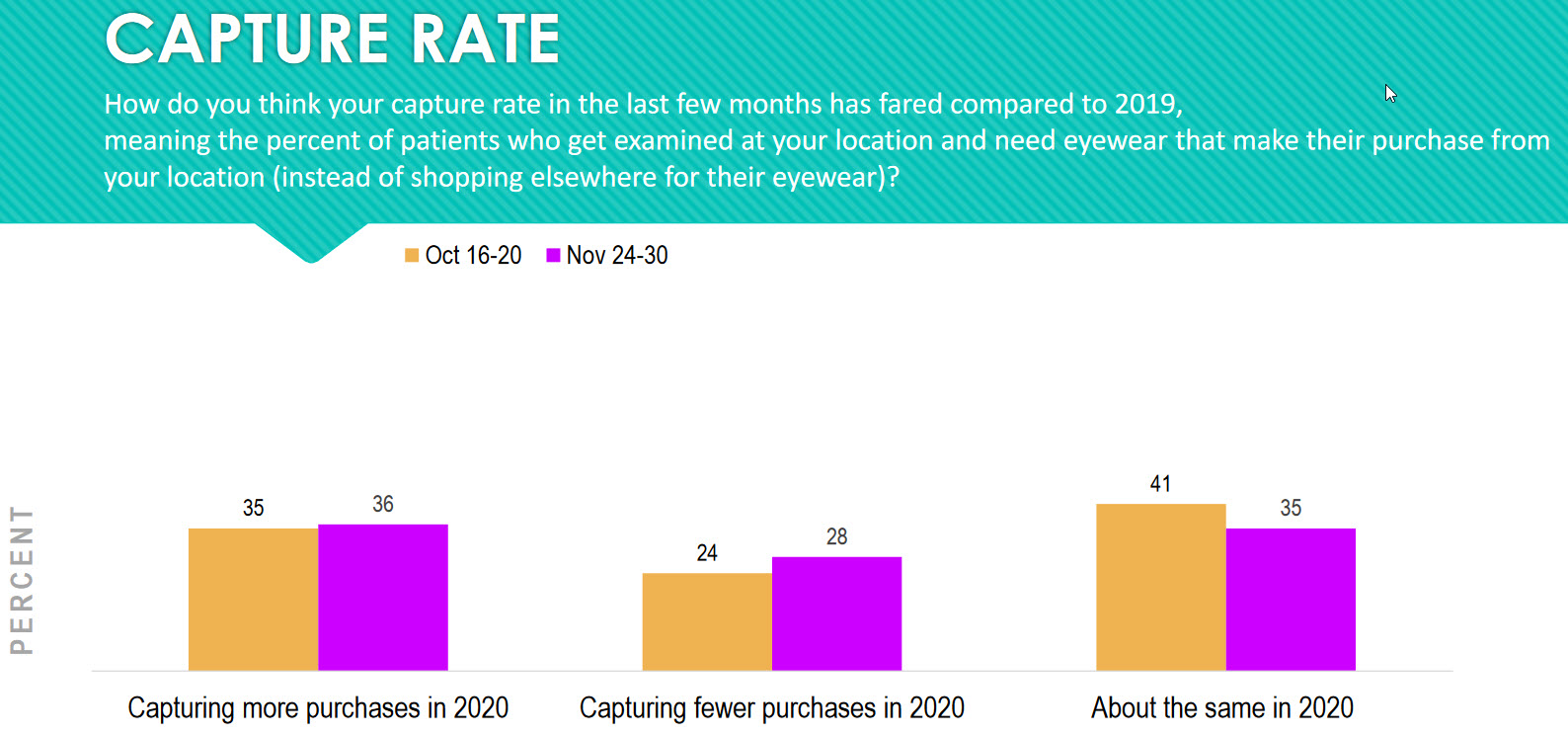
A major key performance indicator (KPI) of a practice is its capture rate. Capture rate is defined in this survey as “The percent of patients who get examined at your location and need eyewear that make their purchase from your location …”
Seventy-one percent (36 percent +35 percent) of practices report their capture rate is either the same or higher than last year. Keep your eye on this number in your practice. Across the country we are seeing a negative dip in this number in some practices (29 percent).
Other Articles to Explore
In the middle of the pandemic, the capture rates in some practices went sky high, and now as we are coming out, the capture rate is returning to a number closer to pre-pandemic. Don’t let this happen to you. Identify best practices and make sure that your staff is following them. It’s too easy to fall into bad habits.
Here are five things to review in your practice to improve your capture rate:
1) Prescribe a solution for each of the patient problems identified.
2) Utilize the best order of presentation of solutions to patients.
3) Train your staff how to handle a “no.”
4) Train your staff to handle objections.
5) Make it easy to do business with your practice.
>>Click HERE to download the latest COVID ECP Impact survey from Jobson Optical Research>>
References
i. Ocular Findings in COVID-19 Patients: A Review of Direct Manifestations and Indirect Effects on the Eye – PubMed (nih.gov)




























