
Kevin Soong, OD, performs diagnostic testing using an OCT in the office of ROB Professional Editor Laurie Sorrenson, OD, FAAO
Coding rules to maximize reimbursement when doing special diagnostic testing.
By Mark K. Davis, OD
Sept. 6, 2023
Having traveled over much of Texas to fill in for optometrists, I have had the opportunity to see the diagnostic equipment that is most common in optometric offices. I am also able to see who the “early adopters” are of the latest pieces of equipment. I don’t believe I have been to any office that doesn’t have at least one piece of special diagnostic equipment. So, let’s dive into special diagnostic testing.
Components
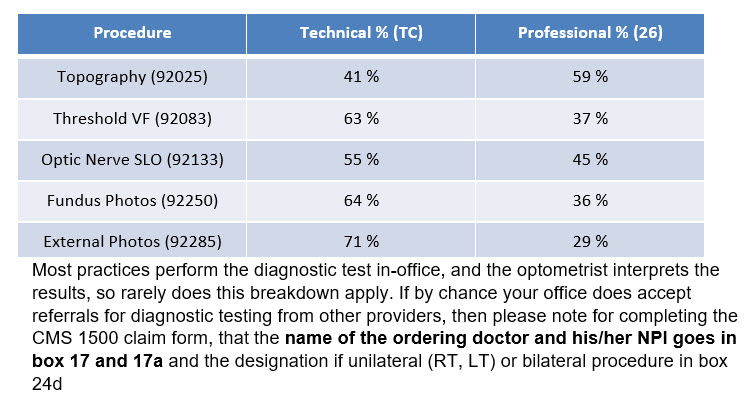
Each diagnostic test has two components:
Technical component (TC modifier) – if your practice just performs the test and sends the results back to the requesting provider for interpretation. There is a percent of the allowable charge.
Examples of the breakdowns of the percentage of the two components on a few common diagnostic tests:
Charting
Each of the diagnostic tests must have (1) a written order in the chart for the special testing, with medical rationale and (2) a separate interpretation and report (there are some exceptions, such as gonioscopy). Refer to the CPT manual for the requirements on each special diagnostic test. It will state in the definition of the test “with interpretation and report,” if one is needed.
An example of a written order could be:
“Order glaucoma evaluation to include OCT, VF, pachymetry, photos and gonioscopy due to several risk factors for POAG”
All the tests need not be performed on the same day, as some cannot be, based on the NCCI edits, covered in a previous article on modifiers. The most common and well known is that you cannot bill for fundus/disc photos (92250) and OCT (92133) on the same day. Again, there are always exceptions. In this case, using the 59 modifier would override the NCCI edit.
Interpretation and Report
So, what is included in the Interpretation & Report? At a minimum the following:
Patient name and date of service
Type of service: visual field or fundus/disc photos or OCT, etc.
Reliability of test: good quality or
technical difficulty, but still adequate or
repeat test required
Findings and Implications: within normal limits or
outside expected limits or
other
Comparative Data: base line exam or
follow-up exam – essentially stable or progression of defect
Management: medication change or
recommend surgery or
further diagnostic testing recommended or
referral
Physician signature & date
For information on CMS guidelines for Interpretation and Report:
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c13.pdf
An Interpretation and Report must be generated for EACH diagnostic test performed. You cannot just scribble your thoughts on the printout from the diagnostic test, to pass an audit. I have seen this many times.
New Diagnostic Test Codes
Two new diagnostic testing codes were added in 2020:
92201
Extended ophthalmoscopy of peripheral retina
With retinal drawings
With scleral depression
99202
Extended ophthalmoscopy of optic nerve & macula
With drawings
No scleral depression
These codes replace codes 92225 and 92226. Also, you cannot bill fundus photos (92250) on the same day as these diagnostic tests.
Many of the EHRs I have used at various offices have tabs and check boxes for Special Diagnostic Testing. Some even remind you to complete the report! This makes reporting exceptionally easy.
Other Articles to Explore
Unlisted Ophthalmological Code
What about a diagnostic ophthalmological procedure that does not have a specific CPT code? Then use CPT code 92499. You must put a description in block 19 and most often you will be denied and have to go through the appeals process. Is it worth your time? One last note, modifiers are not appended to unlisted codes. I racked my brain and the only code I could think of without a CPT I code, which was not included in a comprehensive ophthalmological exam and that did not have a CPT III code, was Contrast Sensitivity. I’m sure there may be others.
Category III Codes (Temporary Codes)
Category III codes exist so data can be collected on emerging technologies, services and procedures. This data is then used to determine whether new Category I codes are needed. The codes end in the letter “t.” No relative value units (RVUs) are assigned to them on a national level, and without a payer policy there is no payment coverage. You should have Medicare patients sign an Advance Beneficiary Notice (ABN). There will be more information on ABNs in a future article.
Until next time…”Happy Coding.”
 Mark K. Davis, OD, is a Therapeutic Optometrist and Optometric Glaucoma Specialist, Diplomate, American Board of Optometry, Adjunct Assistant Professor, University of Houston College of Optometry and Chief of Optometry, 147th Medical Group. He is Lt Col, Texas Air National Guard, Ellington Field JRB, Houston, Texas.
Mark K. Davis, OD, is a Therapeutic Optometrist and Optometric Glaucoma Specialist, Diplomate, American Board of Optometry, Adjunct Assistant Professor, University of Houston College of Optometry and Chief of Optometry, 147th Medical Group. He is Lt Col, Texas Air National Guard, Ellington Field JRB, Houston, Texas.



























