By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

April 7, 2021
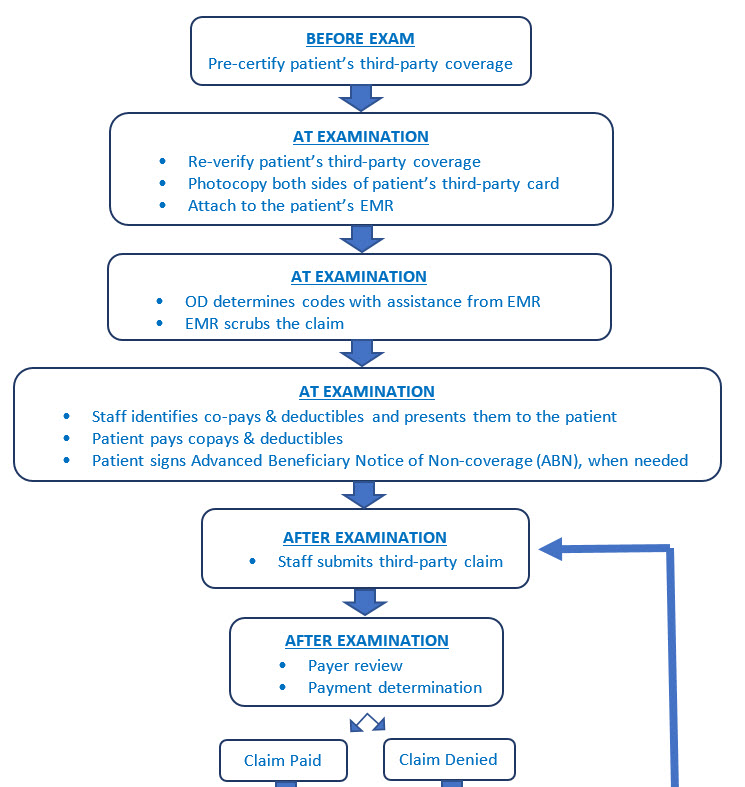
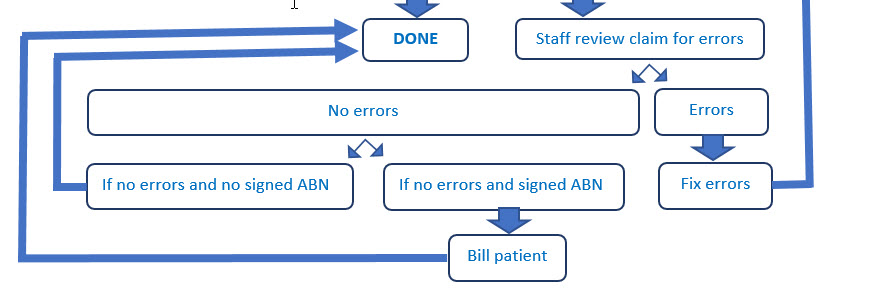
Coding and billing can be intimidating and difficult to track to ensure it is being done correctly every time. Here is a flow chart that will help you put in place a complete coding and billing system to make claim denials less likely and maximize reimbursement.
It is important to create a system for handling third-party claims. This article contains a chart to begin the process. The flow in your office may be different, but the components should be the same.
There are actions that need to be taken before the patient arrives at the office for their exam, actions while the patient is in the office and actions that occur after the patient leaves the office. Be sure to identify them all and educate staff on how important each step is.
The major considerations in the chart are the following:
1) The patient must be pre-certified before they enter the office. It is a terrible mistake for a patient to enter the office ready to have an examination and staff has not pre-certified the patient. What happens when the staff contacts the third-party and they are told the patient no longer has coverage? Often the patient just walks out without an exam. This situation should never be permitted to happen. Pre-certification fixes this.
2) Photocopy both side of the patient’s third-party coverage card. It is essential the patient’s name – exactly as it is spelled on the card – is used for billing. Anything else often results in claim denial.
3) Today’s EHR has the ability to assist in coding by checking to see if the codes chosen match the patient’s record. Use this function, don’t turn it off.
Other Articles to Explore
4) Co-pays and deductibles are due at the time of service. Anything else will grow your accounts receivable and that’s not something you want to do. The other negative for not following this advice is that you have to pay a staff member to track the patient down and try to get payment after they leave the office. No one wants to do that job.
5) Your goal is to submit the claim before the patient leaves the office. Don’t put work off until tomorrow because that just causes the work to snowball. Make it your rule that we don’t go home until all of today’s work is finished.
6) Always review claims for errors. Don’t just accept a third-party denial at face value. Third-parties often make mistakes. Many practices leave a lot of money on the table because they do not reconcile claims and check for errors.
7) An Advanced Beneficiary Notice is only needed when a patient receives either services or products not covered by the third-party. Think of this form as an educational tool. You are communicating to the patient that the following services or materials are not covered by the third-party. We’ve all faced patients who thought that just because they have coverage that everything is covered. This form helps keep misunderstandings to a minimum.
Follow the flow through this form. Is it the same as in your office or do you want to make modifications? If so, make them and then use your modified form to train your staff and to proficiency test them as well.