By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

March 4, 2020
Tracking money coming into the practice, from the first point of contact with the patient, to the last, is essential to profitability. Here is the important role coding and billing play in this process, and how to ensure you are fully reimbursed for all services.
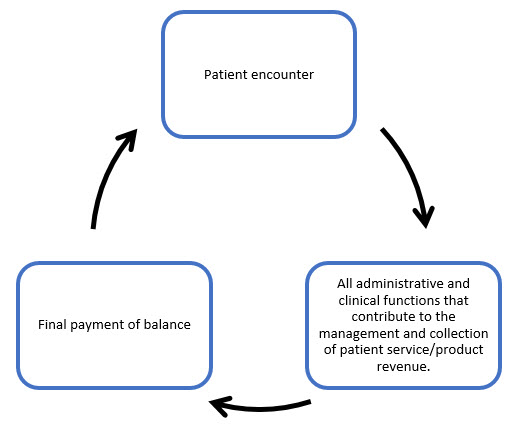
Revenue cycle management is the system that tracks the revenue from patients, from their initial appointment or encounter to the final balance payment. That “cycle” is represented in the graphic below.
The goal of revenue cycle management is to accurately collect the full amount due faster. This system is straightforward when considering a self-paying patient and an office policy of payment at the time of service. The system becomes significantly more complicated when a third party enters the picture. At this point, the rules of the third party play a major role in what you can bill, what you can collect, proper coding and billing, reduction of billing errors so that reimbursements are maximized, what you have to document, what forms need to be filled out, and what time frame you must follow to bill, receive payment and contest a payment.
Here’s an overview of the steps your third-party Revenue Cycle Management system should contain.
REGISTRATION
The first function within the revenue cycle is registration, which allows the provider to obtain all the necessary data needed to properly bill a third party. A key sub-step here is to photocopy the patient’s “insurance” card.
VERIFICATION
Next comes verification. One of the worst scenarios that can occur is for a patient to show up for an exam only to be told that their coverage ended yesterday. This often creates an angry patient and a cancelled appointment. The patient’s coverage should be verified before the patient appears for their exam. Don’t forget to check on the need for prior authorizations. Along with verification of coverage comes clarification of what is covered and what is not. This includes what deductibles and co-pays are due at the time of the examination.
CODING
Next comes coding. A straightforward hierarchy to understand helps clarify this process. The reason for the examination (and medical necessity for medical insurance) determines what testing can be done for reimbursement. Documentation of the testing determines what coding will occur. This step should include a system for clinical documentation integrity – does what was billed match what was documented?
BILLING
Billing is next. Coding determines what billing can happen. Best practices for this step is to utilize a third-party claim scrubbing system to reduce the number of claim denials. Some higher-end practice management systems do this for you. If yours does not, then you can sub this out to a company that will do this for you.
Other Articles to Explore
DENIALS
Handling denials comes next. Just because a third party denies a claim does not mean that the denial is appropriate. You need to know the rules to determine which claims you want to appeal and which denial, if any, can be billed to the patient.
BALANCES
Following up on patient balances comes next. If payment is due at the time of service, then your accounts receivable (AR) should be very low – less than 5 percent of your total AR. If your AR is out of control, then this needs to be addressed immediately.
FINAL PAYMENT
The last step is final payment of balance. When the final payment from all sources for the patient comes in and/or the last denial or appeal has been finalized, then the Revenue Cycle for this patient has been completed and is waiting for the next encounter to begin again.
If we go back to our diagram and fill it out with more detail it now looks like this.

Take this week to review your Revenue Cycle Management system for third parties. Two questions you should ask are: are we receiving the highest level of reimbursement for what is billed and are denials/appeals being managed appropriately? Always look for ways to make your Revenue Cycle Management more effective and more efficient.




























