By Dave Anderson, OD

Oct. 18, 2017
Healthcare is increasingly focused on improved patient outcomes. Achieving successful outcomes often requires a healthcare team working together cooperatively.
My practice co-manages with many primary care doctors for patients with systemic diseases like diabetes and other conditions. An important part of working together is effectively communicating the patient’s current status and medical needs.
We typically have 3-5 new patients sent to us by co-managing MDs per day.
Send Detailed Reports to Co-Managing Doctors
I send letters for nearly everything I find that is relevant to primary care. If I am treating a hordeolum, herpes simplex or corneal disease, the treatment course or the underlying condition may be important to the PCP. No matter the condition, I send a short update letter with the treatment and follow-up details.
There are several conditions that warrant an update regardless of the presence of eye disease. The obvious ones include diabetes and other vascular diseases. I also send letters for any situation where the doctor referred the patient to me, or where they saw me after seeing the PCP, ER or urgent care, but the condition did not improve, so they sought my care.
Don’t Forget to Include the Essential Information
The essential elements, beyond demographics, include the condition, how it is treated and any follow-up care needed. I often include information that would be of value to the PCP, as well. For example, I may be ordering blood work for iritis, and plan to copy the PCP on the order, so they have the results, as well, but I also include why I placed the order.
Use HIPAA-Compliant Mode of Communication
All contact to a patient’s PCP needs to be compliant with HIPAA and privacy laws. That means no communicating about patients via unsecured e-mail, texting and other non-secure methods. The biggest challenge was not just understanding this myself, but also educating my staff, and ensuring they are also compliant.
There are two ways I send letters. The first is via a secure fax and the second is through direct messaging system function of our EHR. As long as the PCP has secured direct messaging, I can e-mail to their EHR for incorporation to the patient’s chart.
Your EHR Can Help Facilitate Communication
The EHR I use has a spot for setting up templates for letter writing. I have many different templates set up for specific reasons. For a diabetic patient, there is a letter for this. For a PCP, I typically send the family doctor an update letter. This automatically populates the information from the exam fields into the letter. While setting up the templates, I choose the chart details I want in each letter, and every time a letter is generated, the chart details are already set up, making for a quick process.
Typically, a letter takes a few seconds, but could be much longer if I have specific details to add. On occasion there are additional tests run, or other details that are necessary to include, that are not in the ready-made template. In those cases, at most, only a few minutes is needed to complete the letters.
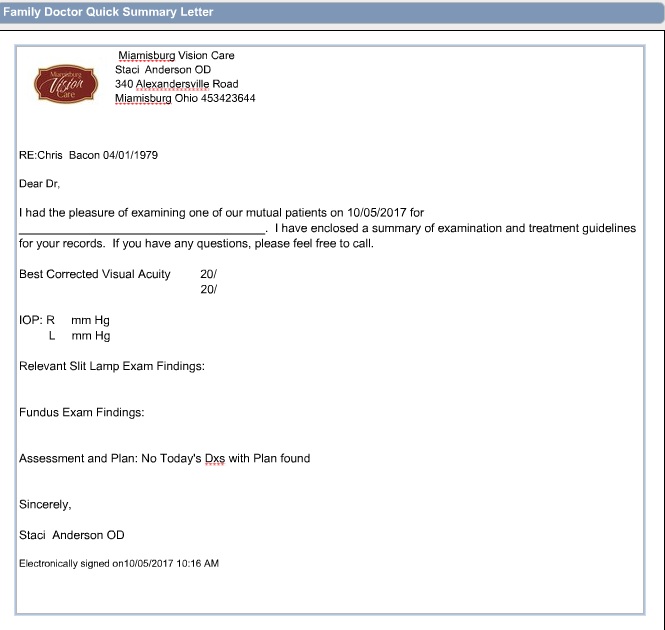
A template for communication with a primary care physician. Dr. Anderson says regular and consistent communication with co-managing doctors is essential to building your practice.
A Follow-Up Call is Needed Sometimes
There are times that I need to follow up with a phone call to the co-managing doctor. This doesn’t happen often, but certainly does occur.
For example, I recently needed to make a follow-up call to a PCP after a medication caused an eye-related side effect for the patient, and another time I needed to call the PCP because I suspected sleep apnea related to my findings. Both times, and many others like these, were welcomed by the PCP, and the appropriate change to the patient’s care was made.
Support Staff Can Help With Co-Managing Communication
Some reports are simple enough to have technicians performing them. In fact, a diabetic patient without retinopathy has a simple template in our EHR that shows the doctor’s follow-up notes, and includes how we viewed the retina, that no retinopathy and no macular edema was present. The other assessments are also included on this letter. This is one that I often delegate to support staff as the letter is complete once the chart is complete, and a simple print-and-send is quite easy.
Share Diagnostic Imaging
I send photos via standard mail for most patients that require photo documents to be sent with their chart or letter. To date, this is the best method to send photos. I also send photos using direct messaging through my secure e-mail from my EHR. This is sent simply as an attachment directly to the doctor intended.
Let Patients Know You Are Communicating with their Primary Care Physician
I like to inform patients of the intention to send letters about their condition to their primary care physician. I include information to this effect in our privacy policy, and in the HIPAA consent forms provided to all patients as they arrive, but more specifically, I have the conversation with each patient when a letter is sent. This does two things, one, it lets the patient know you are taking the time to communicate with their other doctors, and two, it impresses upon the patient the systemic, and potentially serious, implications my findings.
 Dave Anderson, OD, is a partner with Miamisburg Vision Care in Miamisburg, Ohio. To contact: doca@burgvision.com
Dave Anderson, OD, is a partner with Miamisburg Vision Care in Miamisburg, Ohio. To contact: doca@burgvision.com