By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

June 24, 2020
With all states now open for business, people are circulating in your community, increasing the risk for the spread of COVID-19.
Have you made a plan yet for what you will do if one of your employees tests positive? Here are key steps to take if that situation occurs in your office.
The Centers for Disease Control (CDC) issued a report, Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019 (COVID-19), May 2020. Within that report is a section titled Prevent and Reduce Transmission Among Employees. Here are the actions contained in that section of the CDC Guidance.
Actively encourage sick employees to stay home
• “Employees who have symptoms should notify their supervisor and stay home.
• Sick employees should follow CDC-recommended steps. Employees should not return to work until the criteria to discontinue home isolation are met, in consultation with health-care providers.
• Employees who are well, but who have a sick family member at home with COVID-19, should notify their supervisor and follow CDC-recommended precautions.”
People identified with possible COVID arriving at work
• “Employees who appear to have symptoms upon arrival at work, or who become sick during the day, should immediately be separated from other employees, customers and visitors, and sent home.
• Have a procedure in place for the safe transport of an employee who becomes sick while at work. The employee may need to be transported home or to a health-care provider.”
Other Articles to Explore
People identified with possible COVID after arriving at work
“In most cases, you do not need to shut down your facility. If it has been less than seven days since the sick employee has been in the facility, close off any areas used for prolonged periods of time by the sick person:
• Wait 24 hours before cleaning and disinfecting to minimize potential for other employees being exposed to respiratory droplets. If waiting 24 hours is not feasible, wait as long as possible.
• During this waiting period, open outside doors and windows to increase air circulation in these areas.
If it has been seven days, or more, since the sick employee used the facility, additional cleaning and disinfection is not necessary. Continue routinely cleaning and disinfecting all high-touch surfaces in the facility.
Determine which employees may have been exposed to the virus and may need to take additional precautions:
• Inform employees of their possible exposure to COVID-19 in the workplace, but maintain confidentiality as required by the Americans with Disabilities Act.
• Most workplaces should follow the Public Health Recommendations for Community-Related Exposure and instruct potentially exposed employees to stay home for 14 days, telework if possible and self-monitor for symptoms.”
This chart comes from the Public Health Recommendations for Community-Related Exposure.
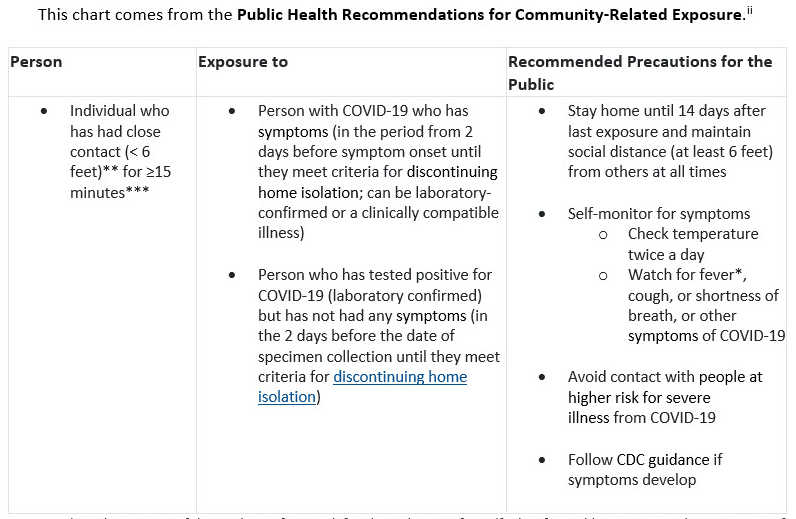 *For the purpose of this guidance, fever is defined as subjective fever (feeling feverish) or a measured temperature of 100.4°F (38°C) or higher. Note that fever may be intermittent or may not be present in some people, such as those who are elderly, immunocompromised, or taking certain fever-reducing medications (e.g., nonsteroidal anti-inflammatory drugs [NSAIDS]).
*For the purpose of this guidance, fever is defined as subjective fever (feeling feverish) or a measured temperature of 100.4°F (38°C) or higher. Note that fever may be intermittent or may not be present in some people, such as those who are elderly, immunocompromised, or taking certain fever-reducing medications (e.g., nonsteroidal anti-inflammatory drugs [NSAIDS]).
** Data to inform the definition of close contact are limited. Factors to consider when defining close contact include proximity, the duration of exposure (e.g., longer exposure time likely increases exposure risk), and whether the exposure was to a person with symptoms (e.g., coughing likely increases exposure risk).
***Data are insufficient to precisely define the duration of time that constitutes a prolonged exposure. Recommendations vary on the length of time of exposure, but 15 minutes of close exposure can be used as an operational definition. Brief interactions are less likely to result in transmission; however, symptoms and the type of interaction (e.g., did the infected person cough directly into the face of the exposed individual) remain important.
Guidance can also be found in the CDC document, “Implementing Safety Practices for Critical Infrastructure Workers Who May Have Had Exposure to a Person with Suspected or Confirmed COVID-19.”
“Critical Infrastructure workers who have had an exposure, but remain asymptomatic, should adhere to the following practices prior to and during their work shift:
Pre-Screen: Employers should measure the employee’s temperature and assess symptoms prior to them starting work. Ideally, temperature checks should happen before the individual enters the facility.
Regular Monitoring: As long as the employee doesn’t have a temperature or symptoms, they should self-monitor under the supervision of their employer’s occupational health program.
Wear a Mask: The employee should wear a face mask at all times while in the workplace for 14 days after last exposure. Employers can issue face masks or can approve employees’ supplied cloth face coverings in the event of shortages.
Social Distance: The employee should maintain six feet and practice social distancing as work duties permit in the workplace.
Disinfect and Clean work spaces: Clean and disinfect all areas such as offices, bathrooms, common areas, shared electronic equipment routinely.”
The overarching important concept is to maintain healthy business operations. Make sure your practice has incorporated these guidance actions into its plan.
References
i. https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html
ii. https://www.cdc.gov/coronavirus/2019-ncov/php/public-health-recommendations.html
iii. https://www.cdc.gov/coronavirus/2019-ncov/community/critical-workers/implementing-safety-practices.html




























