By Whitney Hauser, OD, FAAO

August 26, 2020
Meibomian gland dysfunction (MGD) treatments can offer great benefits to patients in enhanced care, and great benefit to a practice in revenue generation. Here is how to ensure patients say yes to it.
There are now several in-office procedures available for the treatment of meibomian gland dysfunction (MGD). The first of these, LipiFlow (Johnson & Johnson Vision) has been available for nearly a decade, with a strong body of research supporting its efficacy.1-3 Intense pulsed laser (IPL) crossed over from dermatology for use in MGD therapy, and other new entrants to the market include iLux (Alcon), MiBo ThermoFlo (MiBo Medical), and TearCare (Sight Sciences).
When a doctor recommends one of these cash-pay procedures to a patient with MGD, the answer is sometimes “no.” But it’s important to realize that “no” doesn’t have to mean “never”—it just means “not right now.” Here are five ways to reframe your thinking about MGD treatment conversions and increase the chance that patients say “yes” to treatment.
Be Patient with the Learning Curve
In eyecare, “conversion rate” is a LASIK metric that has been applied to anything with a cash-pay component, but there are huge differences between elective refractive surgery and dry eye treatment. MGD patients present with a wide variety of symptoms, ranging from visual fluctuation to tearing or redness. They may not know much about dry eye or MGD, may not yet have accepted that they have a chronic, progressive condition, and almost certainly know very little about treatment options. Their level of readiness to make a decision is several rungs down on the ladder compared to the patient coming in for a LASIK consultation. Give patients time to absorb and process this new information.
Layer it On with Multiple Communications
A layered approach with multiple touch-points is essential to the education process. With EHR systems, we now have the information we need to communicate with patients in a much more targeted way. A few weeks after a new dry eye diagnosis, patients should get a communication from you about the prevalence of dry eye and MGD and common symptoms.
Perhaps a few weeks later, another message could include information about the practice’s treatment options. In other words, you can keep educating patients about relevant topics without inundating them or pressuring them to make a decision. The next time you see them—hopefully in 3-6 months, not a full year—they will be further up the education ladder and more prepared to be receptive to treatment recommendations.
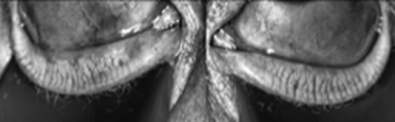
Meibomium glands. Dr. Hauser says you can increase the chances of patients saying yes to MGD treatments with multiple communication touch-points and patient education, among other strategies.
Eliminate the Emotion
Hearing “no” isn’t nearly as satisfying as a “yes” and an immediate conversion. From our perspective as clinicians, we have evaluated the patient, made a diagnosis and offered a solid recommendation for medical care. It can feel insulting or even hurtful to have the patient turn down that recommendation, but it’s important to set aside negative emotions. Resist the temptation to give up on the patient (“OK, just keep doing what you’re doing, Mrs. Smith”) or label them as intransigent. Instead, continue to educate patients about the safety and efficacy of the treatment option you are presenting.
Investigate Whether Staff is Setting You Up for Success
All too often, new technology is introduced to an office with minimal staff education and no incentives or accountability for integrating it into patient care. Conversions become far less likely if the doctor has to do all the heavy lifting in the few minutes he or she has with the patient. I would rather see patients primed for that final conversation by all the interactions they have had with staff leading up to the doctor’s exam.
For example, the front desk staff who hands the patient a questionnaire can plant a seed by saying, “Dr. Hauser would like to know what symptoms you are experiencing so she can contour her care to your needs.” Technicians can educate patients about ocular anatomy, like the meibomian glands (photo to left) and the cornea, and explain the purpose of tests as they go through the workup. That way, patients are less likely to feel that information about their diagnosis and treatment is “sprung” on them at the last minute.
Maybe It’s Not Them, It’s You
Hearing “no” a lot is not necessarily a bad thing. We know that MGD is ubiquitous: 60-80 percent of patients have MGD as a component of their dry eye or contact lens discomfort.4,5 We should all be offering treatment broadly and, as a result, getting some “no” responses. But if “yes” is a rarity, and you’ve already put good staff practices in place, it may be time for a closer look at your own presentation.
Other Articles to Explore
First, make sure you are “reading” the patient and tailoring your message accordingly. The same script won’t resonate with every patient. Some want a lot of detail; others glaze over. Some are scared; others are skeptical or cost-conscious. It can help to do role-playing and scripting. In optometry school, many of us practiced common dialogues about cataract or progressive spectacles. New technology demands the same, so use your staff or people you trust outside the practice to fine-tune how you talk about MGD treatments.
Finally, address the patient who has previously declined treatment with empathy. Here’s how a conversation might go with a patient who opted not to have the procedure I recommended: “I know we decided to do some warm compresses at home…how are those going for you?” The response might be, “Well I started out doing them regularly, but then I went on vacation and kind of forgot to pick it back up.” I would answer, “That’s OK. I’m terrible about doing daily tasks like that myself. You might remember we talked about a procedure called LipiFlow. It takes a few minutes in the office. While the compresses can still be helpful, it won’t be such a big deal if you forget them.”
The bottom line: Continue to address the disease and present solutions. Make it feel right to say “yes” the next time.
References:
1. Blackie CA, Coleman CA, Holland EJ. The sustained effect (12 months) of a single-dose vectored thermal pulsation procedure for meibomian gland dysfunction and evaporative dry eye. Clin Ophthalmol 2016;10:1385-96.
2. Blackie CA, Coleman CA, Nichols KK, et al. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clin Ophthalmol 2018;12:169-83.
3. Greiner JV. Long-term (3-year) effects of a single thermal pulsation system treatment on meibomian gland function and dry eye symptoms. Eye Contact Lens 2016;42(2):99-107.
4. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea 2012;31:472-8.
5. Machalińska A, Zakrzewska A, Adamek B, et al. Comparison of morphological and functional meibomian gland characteristics between daily contact lens wearers and nonwearers. Cornea 2015;34(9):1098-104.
 Whitney Hauser, OD, is the founder of DryEyeCoach.com and Signal Ophthalmic Consulting (SOC). She is in practice at The Eye Specialty Group in Memphis, Tenn., where she focuses on ocular surface disease and surgical management. She is a consultant for Johnson & Johnson Vision, Alcon and Sight Sciences. Contact her at whauser@signalophthalmic.com.
Whitney Hauser, OD, is the founder of DryEyeCoach.com and Signal Ophthalmic Consulting (SOC). She is in practice at The Eye Specialty Group in Memphis, Tenn., where she focuses on ocular surface disease and surgical management. She is a consultant for Johnson & Johnson Vision, Alcon and Sight Sciences. Contact her at whauser@signalophthalmic.com.

























