By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD
ROB Professional Editors

August 2, 2017
Faulty coding can lead to significant lost revenues. Here’s how to determine how much you may be losing, and what to do to correct those errors, and capture greater reimbursements.
Are you leaving $100,000 on the table each year by not coding and billing appropriately? Let’s look at the most common problems that occur in many practices.
CODE TO THE APPROPRIATE LEVEL
Under-coding is just as much insurance fraud as over-coding. Many doctors think if they under-code they reduce their risk for an insurance audit. Nothing could be further from the truth.
Here’s how it works. The software at insurance companies is looking for outliers. An outlier is someone who is coding differently than everyone else. If you are under-coding, then your coding pattern is going to stand out as different, and insurance auditors will want to know why. That means an audit.
“Local doctor charged with fraud and abuse” is not a headline in the local newspaper that leads to practice growth. Code to the appropriate level in all your coding and billing.
BILL FOR REFRACTIONS
Refractions are not part of a CPT-defined medical eye examination. One of the good things the HIPAA law did for us is to say there is one set of rules for coding. For procedure codes, that means the CPT codes. In the CPT codes, 92015 is a separate procedure from the 92000 and the 99000 medical eye examination codes. When you bill a 92000 or a 99000 medical eye examination, if you also do a refraction, then you should also bill a 92015 procedure code.
It is important to understand that Medicare has taken the position that if you do the 92015 procedure, and do not charge for it, you can face discipline.
Here is an interesting question: How much should you bill for 92015? There are two approaches to this question. One approach says to change a small fee like $10. Since the patient will be paying this out-of-pocket, this approach is trying to minimize what the patient has to pay. The other approach says that the refraction may be one of the most important portions of the eye examination, so you should charge a fee equivalent to its importance, such as $100 or more. In both cases, the 92015 refraction fee is in addition to the medical eye exam fee.
COLLECT CO-PAYS & DEDUCTIBLES TODAY
Co-pays and deductibles are due at the time of the examination. Do not wait until you get the Explanation of Benefits (EOB) back from the insurance company to find out how much to bill patients. You should know today what is due from the patient.
There are two reasons that you might not know what co-pays and deductibles are due today.
The first reason is that you (and by extension your staff) have not taken the time to contact the third parties for which you are a provider to find out what the deductibles and co-pays are. Most of the time, these are provided on the insurance card. When that information is not quickly available, a phone call to provider relations often solves this problem. (And, before you complain, yes, provider relations at most third parties, especially Medicare and Medicaid, is often slow and inaccurate but it is the place to start.) Document everything they tell you. Don’t forget to read your provider manual.
The second reason is that the patient does not know how much of their deductible has been met, or it is too much of a hassle to contact the third party to find out how much of the deductible has been met. In today’s world, this should be a simple look-up function on the insurance company’s web site. As a provider, you should have real-time access to this information. Unfortunately, that is not always the case. The solution to this problem is to pre-certify the patient before the eye exam.
Don’t wait until the patient is standing in the office to try to find out what co-pays and deductibles are due today.
Never tell a patient that you will bill them. Billing patients for money they should have paid today causes three problems in the practice: (1) a larger accounts receivable than necessary, (2) waste of staff time chasing patients for money, and (3) loss of money.
When you bill patients instead of having them pay today, you are going to lose money. The longer amount of time that passes before patients pay, the less money you will collect. The graph below shows the dramatic drop off in the amount of money you will collect over time. At 90-120 days, you may only collect 20 cents on the dollar.
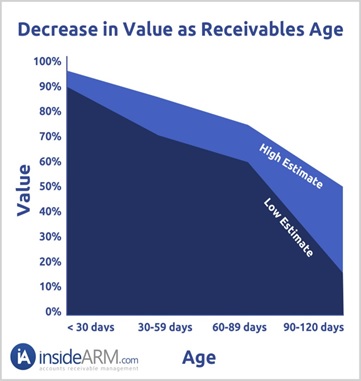
The solution to this problem is to collect what is owed out-of-pocket today.
FOR EMERGENCY EXAMS
When a patient with an emergency presents in your office either during office hours or after office hours, you should bill for the emergency in addition to the services, or procedures, provided. An emergency that occurs during the work day causes disruption to your schedule and inconvenience for all patients who are scheduled after the emergency. An emergency that occurs outside normal working hours causes you to disrupt whatever you were doing and return to the office.
The problem that occurs in today’s world is that many third parties do not pay for emergency codes for optometrists yet we may be required to be on call for emergencies. Does anyone else see the inconsistency in these kinds of policies?
Make sure to have the patient fill out an ABN and sign it as an intake form before you provide the service.
RECONCILE YOUR EOBs
A favorite question we like to ask audiences is: “How many of you have found discrepancies with your third-party payments?” Most, if not all, of audiences raise their hands. That tells you how prevalent the problem is. The next question we like to ask is: “Was the discrepancy in the insurance company’s favor or in your favor?” The overwhelming response is that the discrepancies discovered are in the insurance company’s favor. Few people raise their hands and say the discrepancy was in the practice’s favor. Now you know the bias – and it’s not in your favor.
If you don’t reconcile your EOB, the odds are high you are being underpaid by insurance companies. There is an easy solution to this problem. Reconcile your third-party EOBs to make sure you are being paid according to your contract.
Take this week to review these areas in your coding and billing. Make sure you are being reimbursed appropriately for the work you are doing.

























