By Mark Wright, OD, FCOVD,
and Carole Burns, OD, FCOVD

May 1, 2019
Let’s play a little coding game.
A new patient presents in your office with a medical chief complaint of red eye. This gives you a medical reason for the visit, therefore, potentially the visit can be coded as either a 92000 General Ophthalmolgical Service or a 99000 E/M visit. Let’s see which code set fits the best for this case.
Other Articles to Explore
The following History of Present Illness is taken:
1) Location: Right eye
2) Severity: Mild
3) Duration: Started yesterday
4) Context: Started after playing with the next door neighbor’s cat
Review of Symptoms of Systems gives the following information:
1) Cardiovascular: No rapid heart beat
2) Respiratory: No shortness of breath
3) Gastrointestinal: No upset stomach
4) Genitourinary: Does not go to the bathroom frequently
5) Musculoskeletal: No muscle aches
6) Integumentary: No rashes
7) Neurological: No tingling in the fingers or toes
8) Allergic/Immunologic: Is allergic to cats
For Past, Family, and Social History the following information is documented:
1) Past History: This is the second time this has happened after playing with cats.
2) Family History: No one else in the family is allergic to cats.
3) Social History: The patient likes to dance.
You documented eight physical examination elements.
Your diagnosis is Allergic Conjunctivitis. You are prescribing anti-allergy eye drops.
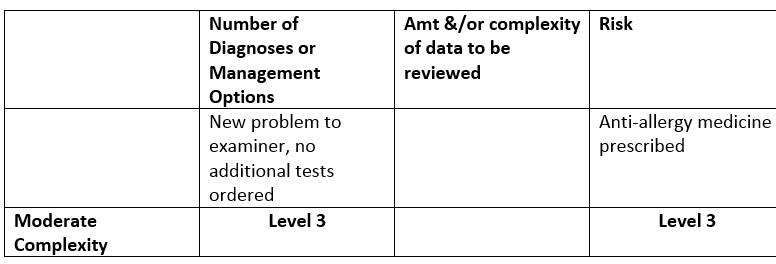
For Medical Decision Making, you documented the following:
So far, this case looks like it could be coded as either a 99000 E/M code or a 92000 General Ophthalmolgical Service. Before we choose which code to use, there are two CPT® code definitions we must keep in mind.
“Comprehensive ophthalmological services describes a general examination of the complete visual system. The comprehensive services constitute a single service entity but need not be performed at one session. The service includes history, general medical observation, external and ophthalmoscopic examinations, gross visual fields and basic sensorimotor examination … It often includes, as indicated: biomicroscopy, examination with cycloplegia or mydriasis and tonometry. It always includes initiation of diagnostic and treatment programs … Initiation of diagnostic and treatment program includes the prescription of medicine, and arranging for special ophthalmological diagnostic or treatment services, consultations, laboratory procedures and radiological services.”
“Intermediate ophthalmological services describes an evaluation of a new or existing condition complicated with a new diagnostic or management problem not necessarily relating to the primary diagnosis, including history, general medical observation, external ocular and adnexal examination and other diagnostic procedures as indicated; may include the use of mydriasis for ophthalmoscopy.”
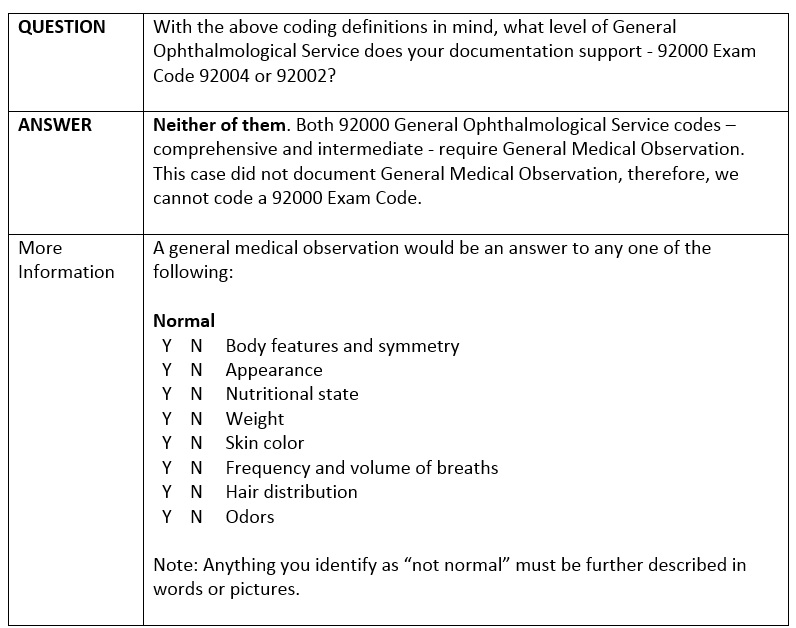
Since we cannot code this patient as a 92000 General Ophthalmological Examination, then we must code the patient as a 99000 E/M visit.
It is important to know the definitions of the codes so that we can follow the coding rules exactly.

























